We don’t usually give our spines much thought – they are simply part of our anatomy. We know they help keep us upright, but that’s about all the attention they get – unless we have back pain. All of a sudden, there’s a spotlight on the spine, and its component parts – vertebrae and discs – are examined. The older we get, the more likely we are to suffer from common spinal issues: bulging or herniated discs.
The Spinal Column: Vertebrae and Discs
In addition to being part of the foundation that supports our bodies’ soft tissues, the spine plays a critical role: it protects the spinal cord, that rope of nervous tissue connecting the brain to other parts of the body, allowing messages to travel throughout our physical structures.
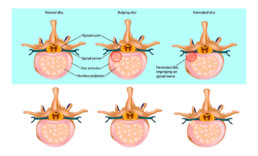
The spinal column has two component parts: vertebrae, the individual, articulated rings of bone that encase the spinal cord; and discs, the cushions that separate the vertebrae and protect them from grinding against each other.
Discs are made up of a fibrous outer layer of tough cartilage surrounding a gel-like centre of soft cartilage. Over time, these discs show evidence of wear and tear. They dehydrate and the cartilage becomes stiff, which can lead to both bulging discs and herniated discs – and potential pain.
Herniated Disc vs. Bulging Disc: Differentiating Disc Difficulties
Often, people assume a disc is a disc is a disc, but there is a difference between a bulging disc and a herniated disc.
A bulging disc results when stiffening causes the outer layer of cartilage to bulge out around its circumference, looking, as the Mayo Clinic describes like “like a hamburger that’s too big for its bun.” The bulge generally affects a quarter or more of the outer layer of tough cartilage.
A herniated disc occurs when a crack in the outer layer of tough cartilage allows some of the softer, gel-like layer to protrude out of the disc. It is also known as a slipped disc or a ruptured disc. The problem is confined to the area around the crack.
Causes of Disc Problems
As noted, discs lose water as we age, becoming less flexible and more prone to dislocating or tearing from bending or twisting. Bad posture can lead to disc issues, as can work that requires repetitive lifting, bending, driving or standing. If you habitually use your back and arms to pick up heavy objects, rather than relying on the power of your lower body, you are at risk.
Risk factors for disc problems include:
- Genetics. Some people are pre-disposed to disc weakness.
- Weight. Additional body weight puts pressure on the discs in your lower back.
- Occupation. People who have physically demanding jobs are at greater risk of disc injury than others.
Symptoms of Disc Issues: Herniated Disc Symptoms
A bulging or herniated disc may produce no symptoms at all – you may never know that you have one. Symptoms generally arise when the problem disc places pressure on nearby nerves or inflames the nerves, causing pain. Common herniated disc symptoms include:
- Pain at the site of the nerve compression.
- Arm or leg pain; when you sneeze or cough, pain may also shoot through these appendages.
- Tingling or numbness in related parts of the body.
- Muscle weakness in the arms or legs, causing stumbling or an inability to hold objects; or
- Muscle spasms.
Treating Disc Problems: Bulging and Herniated Disc Treatment
By avoiding painful positions, following a prescribed exercise regimen and taking pain medication, you should feel better within a few days. When it comes to bulging or herniated disc treatment, your doctor may prescribe physiotherapy as a way of relieving pain and strengthening your body to prevent further injury.
Physiotherapy treatment for bulging or herniated disc may include:
- Active treatment. Active treatment addresses flexibility, posture, strength, core stability, and joint movement and often includes
- Spinal traction. Spinal traction gently separates the spinal bones or vertebrae of the neck and back.
- Flexibility exercises. Ward off stiffness and prepare you for more vigorous movement.
- Hydrotherapy. Water aerobics are preferable to passive treatment, conditioning your body without undue stress.
- Core strengthening. Core muscles assist your back muscles in supporting your spine; if they are weak, there is extra pressure on your back.
- Muscle strengthening. Strong muscles help support your spine and allow you to cope with pain more easily.
- Deep tissue massage. Relieves deep muscle tension and spasms that prevent movement of the muscles in the affected area.
- Hot and cold therapies. Your physiotherapist may alternate these complementary treatments. Heat increases blood flow to the area to help healing and to remove waste by-products. Cold slows circulation to reduce muscle inflammation and pain.
If rest, medication and physical therapy aren’t relieving your herniated disc symptoms, your physician may prescribe surgery to remove the herniated portion of the disc, but this is only necessary in a small minority of cases. He or she may also suggest alternative treatments such as acupuncture, yoga or chiropractic spinal manipulation to relieve ongoing pain.
