With our aging population here in Canada, you may have noticed an increasing number of people walking with canes or limping as they walk. Aging translates to wear and tear on our bodies, and our joints are very susceptible.
One of the most common ailments as we age is osteoarthritis or arthritis of the bones, often called “wear and tear” arthritis. Osteoarthritis can occur in any of our joints, and the hip is one of its most common locations.
A 2009 Statistics Canada survey found that arthritis affects 10 per cent of the Canadian population ages 10 and up. Of those 20 and older, 37 per cent of arthritis sufferers said osteoarthritis was their sole arthritic condition; two per cent experienced hip pain; 29 per cent had knee pain and 29 per cent experienced both. These numbers certainly don’t prompt us to cheer, “Hip, hip, hooray!”
Osteoarthritis Hip Pain Explained
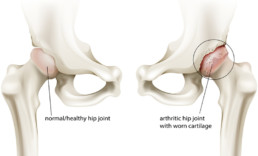
The hip is a ball and socket joint; the head of the upper leg bone, or femur, fits into the socket created by the acetabulum, a section of the large pelvis bone. The surfaces of both bones are generally covered with cartilage, a slippery substance that protects and cushions them. Between the bones, there is also a thin layer called the synovium, which produces fluid to lubricate the cartilage to ensure that movement happens smoothly. The cartilage also helps to absorb any shocks that aren’t dispersed by your hip bones.
With osteoarthritis, the cartilage begins to wear away and becomes rough in the process. The protective space between the two bones shrinks and, without cartilage, the bones may rub against each other. Bone spurs may also pop up, attempting to compensate for lost cartilage. It’s a slow process, but one that is increasingly painful.
Risk Factors
Although the actual cause of hip osteoarthritis and deterioration hasn’t been identified, you are more likely to suffer from it if you have one or more risk factors, including aging; heredity or congenital defects; previous trauma to the joint, such as a broken hip from years earlier or effects of sporting activities; obesity – the hip experiences six pounds of pressure for every pound we gain; and gender – women are more likely than men to experience it.
Osteoarthritis Hip Symptoms
Because hip osteoarthritis is an ailment that develops slowly, people often ignore it until it affects their daily activities. If you have hip osteoarthritis, you may have stiffness in the groin, buttocks or thigh after sitting or lying down for long periods of time, including when you arise in the morning.
You’ll will likely have pain that will worsen over time, especially when you put weight on the hip; it may radiate down the thigh to the knee. You may have some swelling, which can weaken the muscles supporting the joint. Your hip joint may lock or stick periodically and there may be a sensation of bones rubbing against each other – a crunching or popping sensation.
Walking may be painful and you may unconsciously avoid putting weight on the hip, giving your gait a limping or lurching motion. You may have some loss of function – tasks that require bending, such as tying your shoes, may become difficult, and it may be a challenge to get into a car or a chair.
Treatment for Osteoarthritis of the Hip
In addition to discussing your history and doing an examination, your doctor will test your range of motion and check for pain points. He/she may order an MRI or an X-ray to confirm the diagnosis.
It isn’t possible to reverse the damage done to your hip by osteoarthritis, but you can slow its progress and address the symptoms. Relieving pressure on the joint through weight loss and/or muscle strengthening are common approaches. For more severe cases, injections and surgery may be suggested.
Any approach to treatment should aim to reduce pain and ensuring that you can function well enough to carry on with your daily activities. You’ll need to find the proper balance between activity and rest; inaction simply exacerbates the condition. You can also use a cane in the opposite hand and/or wear cushioned shoes to relieve some of the pressure on the hip when walking.
Non-invasive treatment should be your starting point, and physiotherapy is a useful tool to strengthen your surrounding muscles, increase range of motion and reduce pain. Your physiotherapist will start by manipulating your hip, moving on to designing a course of stretching and strengthening exercises.
Osteoarthritis hip exercises can also decrease stress on the hip and increase stability. They may also help you modify your gait. You’ll want to minimize activities, such as running, that cause pain and try those, such as swimming, that don’t place stress on the hip.
More Invasive Treatments
You may also consider more invasive options. Your physician may suggest steroid injections to reduce swelling or hyaluronic acid injections that provide lubrication to the joint to make movement easier. They don’t work equally well for everyone, but if they are successful, the impact lasts anywhere from six months to a year.
Surgery is the most drastic response to hip osteoarthritis. If the osteoarthritis is having a major impact on your lifestyle, you may want to consider it. There is arthroscopic surgery that can be used to remove bone spurs or loose pieces of cartilage; osteotomy that reduces friction by aligning bones properly; and total hip replacement, which replaces your joint with an artificial one. Discuss these possibilities with your physician if the osteoarthritis becomes severe.
Finally, don’t take your condition lying down (you’ll get stiff!). Be proactive in addressing it by staying active, losing weight and adopting a course of exercise that will strengthen the muscles around the hip.
