Herniated Disc vs. Bulging Disc
We don’t usually give our spines much thought – they are simply part of our anatomy. We know they help keep us upright, but that’s about all the attention they get – unless we have back pain. All of a sudden, there’s a spotlight on the spine, and its component parts – vertebrae and discs – are examined. The older we get, the more likely we are to suffer from common spinal issues: bulging or herniated discs.
The Spinal Column: Vertebrae and Discs
In addition to being part of the foundation that supports our bodies’ soft tissues, the spine plays a critical role: it protects the spinal cord, that rope of nervous tissue connecting the brain to other parts of the body, allowing messages to travel throughout our physical structures.
The spinal column has two component parts: vertebrae, the individual, articulated rings of bone that encase the spinal cord; and discs, the cushions that separate the vertebrae and protect them from grinding against each other.
Discs are made up of a fibrous outer layer of tough cartilage surrounding a gel-like centre of soft cartilage. Over time, these discs show evidence of wear and tear. They dehydrate and the cartilage becomes stiff, which can lead to both bulging discs and herniated discs – and potential pain.
Herniated Disc vs. Bulging Disc: Differentiating Disc Difficulties
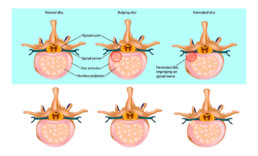
Often, people assume a disc is a disc is a disc, but there is a difference between a bulging disc and a herniated disc.
A bulging disc results when stiffening causes the outer layer of cartilage to bulge out around its circumference, looking, as the Mayo Clinic describes like “like a hamburger that’s too big for its bun.” The bulge generally affects a quarter or more of the outer layer of tough cartilage.
A herniated disc occurs when a crack in the outer layer of tough cartilage allows some of the softer, gel-like layer to protrude out of the disc. It is also known as a slipped disc or a ruptured disc. The problem is confined to the area around the crack.
Causes of Disc Problems
As noted, discs lose water as we age, becoming less flexible and more prone to dislocating or tearing from bending or twisting. Bad posture can lead to disc issues, as can work that requires repetitive lifting, bending, driving or standing. If you habitually use your back and arms to pick up heavy objects, rather than relying on the power of your lower body, you are at risk.
Risk factors for disc problems include:
- Genetics. Some people are pre-disposed to disc weakness.
- Weight. Additional body weight puts pressure on the discs in your lower back.
- Occupation. People who have physically demanding jobs are at greater risk of disc injury than others.
Symptoms of Disc Issues: Herniated Disc Symptoms
A bulging or herniated disc may produce no symptoms at all – you may never know that you have one. Symptoms generally arise when the problem disc places pressure on nearby nerves or inflames the nerves, causing pain. Common herniated disc symptoms include:
- Pain at the site of the nerve compression.
- Arm or leg pain; when you sneeze or cough, pain may also shoot through these appendages.
- Tingling or numbness in related parts of the body.
- Muscle weakness in the arms or legs, causing stumbling or an inability to hold objects; or
- Muscle spasms.
Treating Disc Problems: Bulging and Herniated Disc Treatment
By avoiding painful positions, following a prescribed exercise regimen and taking pain medication, you should feel better within a few days. When it comes to bulging or herniated disc treatment, your doctor may prescribe physiotherapy as a way of relieving pain and strengthening your body to prevent further injury.
Physiotherapy treatment for bulging or herniated disc may include:
- Active treatment. Active treatment addresses flexibility, posture, strength, core stability, and joint movement and often includes
- Spinal traction. Spinal traction gently separates the spinal bones or vertebrae of the neck and back.
- Flexibility exercises. Ward off stiffness and prepare you for more vigorous movement.
- Hydrotherapy. Water aerobics are preferable to passive treatment, conditioning your body without undue stress.
- Core strengthening. Core muscles assist your back muscles in supporting your spine; if they are weak, there is extra pressure on your back.
- Muscle strengthening. Strong muscles help support your spine and allow you to cope with pain more easily.
- Deep tissue massage. Relieves deep muscle tension and spasms that prevent movement of the muscles in the affected area.
- Hot and cold therapies. Your physiotherapist may alternate these complementary treatments. Heat increases blood flow to the area to help healing and to remove waste by-products. Cold slows circulation to reduce muscle inflammation and pain.
If rest, medication and physical therapy aren’t relieving your herniated disc symptoms, your physician may prescribe surgery to remove the herniated portion of the disc, but this is only necessary in a small minority of cases. He or she may also suggest alternative treatments such as acupuncture, yoga or chiropractic spinal manipulation to relieve ongoing pain.
Let's get you some relief from your pain!
Tennis Elbow and Golfer’s Elbow
“Summertime, and the livin’ is easy,” says the old song. School is out, vacations are on the calendar and the weather is conducive to all sorts of outdoor activities. For summer sports enthusiasts, it’s a treat to be able to leave the gym behind and head out to the tennis court or the golf course – unless, of course, injury makes that impossible. For avid tennis players and dedicated golfers, there’s always the danger of an overuse injury such as tennis elbow or golfer’s elbow.
What is Tennis Elbow?
With tennis elbow pain results from repeated contraction of the forearm muscles that you use to straighten and raise your hand and wrist. How do you get tennis elbow? When playing tennis, you may grip the racquet too tightly or use poor technique, putting stress on the tendons connecting your muscles to your elbow bone. Other activities can also lead to overuse and injury, including:
- Cutting up ingredients for cooking, particularly meat
- Repetitive computer mouse use
- Using plumbing tools
- Painting
- Driving screws
What are some of the tennis elbow symptoms? With tennis elbow, pain generally radiates from the outside of your elbow to your forearm and wrist. It may make it challenging for you to hold a coffee cup, shake hands or turn a doorknob.
What is Golfer’s Elbow?
Golfer’s elbow generally results from overusing the muscles in the forearm that allow you to grip, rotate your arm and flex your wrist. The repetition required by gripping and swinging can injure the tendons in your forearm that attach to your elbow. Other athletes, such as pitchers and bowlers are also prone to golfer’s elbow, and it can result from regular hammering, raking and painting, too.
Golfer’s elbow results in tenderness and pain on the inside of your forearm. You may also feel stiffness in your elbow, making it difficult to curl your fingers into a fist. Your hands and fingers may feel weak and there may be a tingling sensation that radiates into your fingers. You may find it challenging to pick up something with your palm facing down or to flex your wrist.

How do you treat Elbow Pain?
Let’s discuss how to treat tennis elbow and golfers elbow. Both usually respond to self care. Most commonly the treatment for tennis elbow and golfer’s elbow is as follows:
- Take a break. Give your golf or tennis game a rest until the pain disappears. It may be frustrating, but returning to action too soon may cause the injury to recur.
- Cold comfort. Ice the injured area for a few days to provide relief and reduce any inflammation. Try icing the elbow a few times a day for 15 to 20 minutes, using a pack wrapped in a dishtowel so the ice doesn’t injure your skin. The injured tendons lie close to the skin, so they don’t need long icing sessions.
- Brace yourself. Wearing a specialized elbow brace can provide support that reduces the strain on the tendon, allowing it to heal.
- Rub a dub dub. You may want to massage the affected area for five minutes at a time once the inflammation has disappeared.
- Mouth to hand relief. You may want to use an over-the-counter pain reliever to alleviate some of the pain.
If the injury doesn’t seem to be healing, you may want to consult further with your physician. He or she will probably suggest:
- Physiotherapy. Stretching and strengthening the affected area will promote healing while preventing further injury. Eccentric exercises, which lengthen the tendons, have proved to be effective. Your physiotherapist may also use ultrasound or electrotherapy to reduce pain and assist with healing.
- Injections. A new therapy involves injecting platelet-rich plasma into the affected area to hasten healing.
- Surgery. If there is no improvement within six months to a year, it is possible to have the damaged tissue surgically removed.
What is the main cause of Tennis Elbow and Golfer’s Elbow?
Both tennis elbow and golfer’s elbow are repetitive stress injuries caused by overuse that result in inflammation and small tears to tendons in the arm. Tendons connect muscle to bone. Tennis elbow – lateral epicondylitis – refers to injury to tendons on the front of the arm, while golfer’s elbow – medial epicondylitis – is the name given to injury to a forearm tendons.
How log does it take to recover from Tennis Elbow or Golfer’s Elbow?
You shouldn’t return to tennis or golf – or the other activities that led to the injury – until you can perform the challenging motions without pain. Don’t rush yourself, or you will simply re-injure the tendons.
Return to activity gradually. You may want to wear an elbow brace to start, and it is wise to consult with a professional to ensure that you are using the proper motion. If you feel pain during or after exercise, back off for a while. The goal is to stay healthy.
We offer Physiotherapy for Tennis and Golfer's Elbow!
Ankle Sprain and Instability
You’ve undoubtedly seen it happen while watching a basketball game: a player jumps to grab a rebound and turns his foot as he lands awkwardly on his ankle. The player limps from the court, seeking help from the trainer. Ouch!
What the player has suffered is a sprained ankle. Everyone is familiar with the term, but what does it actually mean?
Ankle Sprains Explained
An ankle sprain is one of the most common injuries to the soft tissue of the ankle. It is estimated that approximately 100,000 Canadians suffer ankle sprains annually. In college and university sports, it is one of the most common injuries among both men and women.
An ankle sprain occurs when the ligaments, the bands of fibrous tissue that keep the ankle in place, are stretched or torn. It generally happens when the ankle is twisted, which can happen during an intense activity, such as a sport, or by simply losing your balance or stepping onto an uneven surface while walking.
A mild sprain results when the ligaments are simply stretched, a severe sprain occurs when the ligaments actually tear.
Sprained Ankle Symptoms
If you sprain your ankle, you can expect one or more of these symptoms:
- Pain.
- Bruising, resulting from ruptured blood vessels leaking into the tissue.
- Swelling, resulting as fluid continues to leak into the tissue for 24 hours after the injury.
- Tenderness when touched.
- Joint instability, especially if the ligament is torn through.
- A possible popping sound.
A severe sprain will exhibit symptoms similar to those of a broken bone and should receive immediate medical evaluation.
Diagnosis
During a physician’s physical examination of your ankle she or he will:
- Palpate. Gently press the area around the ankle to determine which ligaments are affected.
- Test range of motion. Move the foot in various directions to see which movements are possible.
- Use imaging. Images of your ankle may assist in diagnosis. X-rays can determine whether any bones are broken, while an ultrasound allows for observation as the ankle moves to see how much stability the ligament offers. Magnetic Resonance Imaging (MRI) may be used once swelling recedes to determine the extent of the injury.

Classification
Sprains are graded based on their severity – the amount of damage done to the ligaments. Grading is helpful to physiotherapists when they treat patients with sprains.
Grade 1 ankle sprain – mild
- Ligaments are stretched slightly and there may be microscopic tears.
- There is mild swelling, bruising and tenderness around the ankle.
Grade 2 ankle sprain – moderate
- The ligament is partially torn.
- Tenderness, bruising and swelling around the ankle are moderate.
- Ankle is abnormally loose if moved in certain directions.
Grade 3 ankle sprain – severe
- The ligament is torn through.
- Swelling, bruising and tenderness around the ankle are severe.
- With certain motions, there is substantial instability; unable to bear weight.
How to Heal a Sprained Ankle
Luckily for the injured, almost all sprained ankles can heal without surgery. However, healing will take time.
It is important not to treat a sprain lightly, because once an ankle has been sprained, it is more prone to further sprains. You may also experience stiffness and pain. Without proper rehabilitation, you may experience instability, which can lead other muscles to compensate. As a result, your gait may change, placing undue stress on your legs, knees or hips and making them more prone to injury.
Just as there are three grades of sprains, there are three basic steps to any ankle sprain treatment:
- Step 1: Rest, protection of the ankle and swelling reduction.
- Step 2: Restoring strength, flexibility and range of motion.
- Step 3: Maintenance exercises and a gradual return to sports.

Physiotherapy for Ankle Spain
Initially, any sprained ankle can be treated using the RICE method: rest, ice, compression and elevation. However, once the initial swelling has receded, it’s time to turn to a physiotherapist for a rehabilitation program that focusing on rebuilding strength, restoring flexibility and range of motion and promoting stability.
In addition to a series of targeted exercises, your physiotherapist may employ a hands-on treatment called joint mobilization to restore the gliding motion to the ankle bones. Your exercises may also home in on your sense of position or proprioception. Nerve sensors inside your ligaments may be affected during a sprain and they may not give your brain an accurate reading of how your ankle is positioned. You may need to retrain your sense of position as you heal.
How Long Does it Take a Sprained Ankle to Heal?
Sprains generally heal in three to eight weeks if given proper treatment, so handle with care!
Take proper care of your Ankle Sprain!
Achilles Tendon Problems
In Greek mythology, Achilles was the son of King Peleus, a mortal, and a sea nymph, Thetis, and the greatest warrior of the Trojan War. His mother attempted to render him invulnerable by dipping him in the River Styx, protecting his body except for the heel by which she held him for the dipping: his Achilles heel.
Our own Achilles tendons are the strong bands of fibres that connect our calf muscles to the heel. As legend implies, they are, indeed, vulnerable to injury. These injuries generally happen when you begin moving suddenly, pushing off with your foot. Achilles tendinitis (or tendonitis) and a ruptured Achilles tendon are the most common injuries to this tendon.
What is Achilles Tendinitis?
Achilles Tendinitis is an overuse injury due to repetitive motion that can cause pain, inflammation or degeneration of the tendon. It is common among runners and jumpers.
Achilles tendinitis can result from:
- Increasing the duration or intensity of your runs.
- Playing sports only on the weekends in middle age.
- Sudden change in your training surface (e.g., asphalt to grass).
- Flat feet that over-pronate.
- Feet with high arches and tight Achilles tendons.
- Tight hamstrings and calf muscles.
- Shoes without enough support.
Signs and symptoms
- Achilles tendinitis usually starts with mild pain after exercise that requires repetitive motion. You’ll generally feel a mild ache in the back of the leg or heel afterward.
- During the night or when you awaken in the morning, you may feel more pain and stiffness.
- If inflammation is involved, the area may be red, swollen, tender or warm.
- Use of the tendon may result in a crunchy feeling.
Diagnosis: Your physician will examine your ankle and your foot and assess the range of motion and the condition of the tendon. X-rays or other types of imaging may be used.
Achilles Tendinitis Treatment
Once your achilles tendinitis is diagnosed by a doctor, a visit to the physiotherapist is generally in order. Here’s what to expect for your Achilles tendinitis treatment:
- Your pain threshold will be assessed and any movements that cause increase pain identified.
- If there is inflammation involved, your physiotherapist may use ultrasound to reduce it and stimulate blood flow, which promotes healing.
- Deep massage to improve flexibility and further increase blood flow.
- Stretching and flexibility exercises that can assist in healing without shortening the tendon.
- Strengthening exercises to protect against further injury while helping your regain any strength that has been lost.
- Additional support: Your physician may suggest orthotics to elevate your heel, relieve strain on the tendon and lessen the amount of force it absorbs during exercise.

Recognizing an Achilles Tendon Rupture
What is an Achilles tendon rupture? A rupture is a tear in the Achilles tendon when an abrupt movement is too much for the tendon to handle. It can occur spontaneously, without warning, or you may have experienced tendinitis previously.
Achilles Tendon Rupture Symptoms
- You may feel a sudden, sharp pain above your heel as the tendon releases the calf muscle.
- There may be a popping or snapping sensation.
- The back of the leg between heel and calf may swell.
- You’ll have difficulty walking, especially up stairs or uphill.
Diagnosis: A physician or surgeon will ask about your history and the circumstances surrounding the injury. A physical exam will include an evaluation of range of motion and muscle strength, comparing it to the uninjured foot. The diagnosis is usually straightforward, but imaging tests may be required.
Treatment
Immediately after the injury, use the RICE method of treating your achilles: rest, ice, compression and elevation.
Non-surgical option for a ruptured achilles tendon:
- Minor or partial ruptures.
- Less active patients.
- Patients with medical conditions that prevent surgery.
- Employs a cast, walking boot or brace with a heal lift to support the tendon and allow it to heal.
Archilles rupture surgery:
- Decreases likelihood of another rupture.
- May improve push-off strength.
- Generally improves muscle function and ankle movement.
- Requires an incision and stitching the tendon back together.
Achilles Rupture Recovery
Healing from surgery usually takes four to six months. Effort is required to restore your heel to health. Your physician will generally recommend physiotherapy to:
- Strengthen the tendon.
- Regain flexibility.
- Improve agility.
Post-Recovery
Take things slowly. Don’t return to your previous level of physical activity until:
- Your healed leg feels as strong as your other leg.
- You can move your healed leg as freely and easily as your other leg.
- You feel no leg pain when you walk, run and sprint.
An Achilles tendon injury is treatable, so don’t despair.
Are you experiencing problems with your Achilles?
Plantar Fasciitis – Heel Pain
We all have our metaphorical Achilles heels, but for people suffering from plantar fasciitis, the heel itself is actually their weak spot.
What is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the tough, fibrous band of tissue that runs across the bottom of your foot, connecting your toes to your heel. If you took Latin in school, you’ll recognize the terms: plantar refers to the bottom of the foot; fascia means bandage or band; and it means inflammation. It all adds up to an unpleasant injury.
What is the best treatment for Plantar Fasciitis?
Ninety per cent of plantar fasciitis cases can be treated successfully without surgery. There are a variety of techniques that your physiotherapist and physician may recommend, and it may take some time to find the combination that helps you heal and alleviates your pain. The non-invasive possibilities include:
- Ultrasound, soft tissue massage and/or icing. These remedies help decrease pain and inflammation.
- Iontophoresis. Using a mild electric current to push the anti-inflammatory medication that your doctor prescribes into the painful area.
- Exercises. Stretches designed to improve the flexibility in your calves, plantar fascia and Achilles’ tendon.
- Orthotics. These customized arch supports help cushion your heel and support your arch.
- Heel cup. This shoe insert adds support to a heel that has lost some of its fat pad through degeneration.
- Night splint. A splint that you wear while you sleep that prevents your foot from moving into an improper position while you sleep and stretches your calf muscles a bit.
- Taping. You’ll see athletes using this method to provide temporary relief to sore parts.
If your pain isn’t lessening after a few months, a professional may suggest one of these measures:
- Injections. Injecting steroid medication into the sore area may provide temporary pain relief. However, this shouldn’t become an ongoing solution because it can weaken the fascia.
- Extracorporeal shockwave therapy. Sound waves target the painful area to relieve pain. This is used largely for chronic cases and may cause side-effects, such as swelling, numbness and tingling.
- Surgery. As a last resort, surgery can detach the fascia from the heel bone, but it does weaken the arch in the foot.

What is the main cause of Plantar Fasciitis?
The plantar fascia is made up of collagen fibres. When you put your foot on the ground, you are placing a great deal of force on these fibres as your foot tries to flatten. The force stretches the fibres and it can lead to tears and bleeding on the band where it attaches to the heel bone.
Plantar fasciitis affects men and women of all ages, athletic or not. Factors that influence susceptibility include:
- The calendar. It is most common between the ages of 40 and 60.
- Change of pace. A rapid increase in the length or difficulty of activity (e.g., a new job that requires you to be on your feet much more than you were previously).
- Foot mechanics. Flat feet, high arches or an unusual walking pattern can affect the way your weight is distributed when you’re standing.
- Heavy hitters. Increased body weight with a body mass index greater than 30; extra pounds place additional stress on your feet.
- On your feet. A job, hobby or sport that requires prolonged standing or other weight-bearing activity – think of teachers and factory workers, for example.
- Tightening. A decrease in the flexibility of your calf muscles.
- Flimsy flats. Wearing shoes with inadequate support.

Plantar Fasciitis Symptoms
If you experience any of the following symptoms, there’s a chance you’re suffering from plantar fasciitis and it’s time for a visit to your physiotherapist:
- Pain on the bottom of your heel or along the inside edge near the arch.
- Heel pain that increases over a period of months.
- Pain that returns after you spend a long period of time on your feet.
- Pain that radiates into your arch, the side of your heel or up the back of your leg.
- Pain that is worse when you get out of bed in the morning; the first few steps may be agonizing.
- Your heel may feel better after you exercise, but it usually returns by the end of the day.
- Pressing on the heel causes tenderness, while pulling your toes back toward your face can be very painful.
- Heel pain when climbing stairs or walking barefoot.
Don’t become one of the victims of plantar fasciitis. Preventive measures include stretching before and after running or walking; maintaining a healthy body weight; and wearing shoes with good arch support. However, if you do experience heel pain, it’s important to know that relief is possible.
Is Plantar Fasciitis causing you Heel Pain?
Why Do Muscles Feel Tight?
We’ve all experienced the unpleasantness of stiff or sore muscles, whether they feel tight when we get out of bed in the morning or after a long walk or run. Even if the pain isn’t excruciating, the stiffness can be frustrating. In fact, it may tempt us to forego our exercise sessions, which isn’t healthy in the long run.
Why do we feel these sensations, and what are our bodies trying to tell us?
Why tightness?
Our muscles expand and contract as we exercise, and we feel stiff when the muscle fibres contract, seize up and find it difficult to expand. Here are some situations where that may occur:
- Missing minerals. Muscles need magnesium to relax and calcium to tighten. If the two aren’t in balance, muscles can contract or have spasms.
- High and dry. Muscles, which are active tissues, require water to function properly. Water contains the electrolytes that send messages between the nervous system and the muscles. When the proper amount of water is lacking this communication ability is impaired and muscles don’t work smoothly.
- Genetics. Muscles have both slow twitch and fast twitch fibres. Fast twitch fibres don’t consume oxygen and are most likely to stiffen. Most people have the same amount of each type of fibre, but if you have an excess of fast twitch fibres, you may be more prone to stiffness.
- Inactivity and imbalance. During prolonged periods of inactivity, muscles may tighten due to their restricted movement. For example, when you sit too long, the hip flexors (front hip muscles) tighten and the gluteal muscles (rear hip muscles) lengthen, causing an imbalance. The tightened muscles may feel stiff, while the lengthened muscles may weaken. Balance is the key for the long term.
- Short, but not sweet. Your muscles may tighten – i.e., cramp – while you are exercising. When your muscles contract, the fibres shorten and tension in the muscle increases. When the contraction finishes, the fibres decrease the tension and lengthen. A cramp occurs when the fibres are unable to lengthen. The ongoing shortened muscles may be due to fatigue, poor hydration or inadequate nutrition.
- Home and cooled out. Tightness, which is experienced as soreness, may be felt for 24 to 72 hours after exercise as a result of small ruptures in your muscles. It is most common after doing exercises that involve contractions where a weight is lowered.
What Relieves Muscle Tightness?

Using non-steroidal anti-inflammatory drugs reduce inflammation and pain, but they may actually slow the healing process. A post-exercise massage may be more beneficial.
Vigorous exercise causes tiny tears in muscle fibres and inflammation is the immune reaction signalling that the body is working to repair these tears. Compounds called cytokines are involved in inflammation, and they are reduced by massage. Massage also stimulates the mitochondria inside the muscle cells; these mini-machines turn glucose into the energy necessary for cell repair and functioning.
Massage is also a good remedy for muscle tightness for other reasons:
- Blood flow. Massage improves circulation and blood flow is important in healing muscle tears, because it carries nutrients necessary for muscle repair.
- Sleep therapy. Sleep is part of the recovery process, and massage can improve the quality and quantity of the athlete’s sleep.
Preventing Muscle Tightness from Occurring

- Watch your posture. Be aware of positioning when you are seated and when you sleep, ensuring that you’re not overloading particular muscles, leading to tightness.
- Strengthen muscles prone to tightness. Strong muscles take longer to tighten, since they are able to handle the work they are given. Weak muscles are more likely to get tight.
- Don’t neglect adjacent muscles. One muscle may get tight because it is required to do the work of a weak muscle next door. Don’t allow that to happen.
- Get moving. Staying in one position for any length of time, even if it’s a proper one, isn’t good for you. Moving around every so often will prevent muscles from getting tight.
The message in a nutshell? Stay loose, folks, but if you can’t, consider a massage from a Registered massage therapist!
Experiencing MUSCLE TIGHTNESS or TENSION?
Coping With Neck Pain and Headaches
How many times have you thought of somebody to be “a pain in the neck”? Interestingly, however, a number of physical issues that affect the neck actually manifest themselves as “a pain in the head” – or a headache. There are many causes of neck pain and of headaches, so make sure you are informed before you decide upon a course of treatment – get a diagnosis from your physician or physiotherapist.
How to Relieve Neck Pain
Physiotherapists are trained to diagnose and treat neck joint dysfunctions and muscle imbalances. Your physiotherapist may employ some or all of the following techniques, depending on the individual diagnosis of your neck pain:
- Gentle join mobilization and manipulation to loosen or unlock stiff neck joints.
- Strengthening exercises for weak muscles, focusing on neck muscles and postural shoulder blades.
- Stretching, massage, acupuncture, dry needling or other relaxation techniques to provide relief to tight or overactive muscles.
- Deep neck muscle strengthening exercises for control, stabilization and limiting the joint movement of unstable joints.
- Exercise, awareness, taping or a brace to correct poor posture.
- Prevention advice regarding awkward postures to avoid in future.
In addition, if you have any type of nerve dysfunction, it will be addressed with special care. Depending upon the severity of your problem and its underlying causes, it should be resolved within a few days or a few weeks. Rehabilitation will be based on both treatment and prevention.
Why Does my Neck Hurt?
Although the physical problem originates in the neck, the pain radiates to the head, causing discomfort; the pain signals travel from your neck to the trigeminocervical nucleus in your brainstem and a headache results. Research has shown that neck headaches account for anywhere from 4% to 22% of all headaches treated clinically.
Various musculoskeletal or neurovascular structures in your cervical spine (neck) can be at the root of cervicogenic neck headaches when they are out of balance or malfunctioning. Your neck joints, neck muscles and nerves are the most likely culprits of your neck pain.
- Your joints may be too stiff or too wobbly – unsupported because surrounding muscles are weak.
- The joints may also be locked in an abnormal joint position, likely due to poor posture. Given the number of us who sit in front of computer terminals all day, this shouldn’t be surprising.
- Problems with your cervical disks may also result in pain that radiates from neck to head.
Your neck muscles may work too hard if they are trying to protect injured joints. Over time the balance in your neck muscles changes, causing your head to feel heavy because some of the muscles that should be supporting your head have weakened, while the others have tried to compensate. Neck muscles work best when they have normal resting tension, length, strength, power and endurance.

Common Neck Headache Symptoms
If you are experiencing one or more of these symptoms, you likely have a neck headache:
- Tenderness at the base of the skull and top of the neck.
- Neck stiffness or mild loss of movement.
- Your headache pain radiates from the back of the head to the front.
- Your headache is centred on one side of your head or the other and stays there.
- When you apply pressure or massage the base of your skull or your neck, the pain eases.
- Your headache is lessened or heightened by a sustained posture, neck movement, or sleeping on your stomach or with your head turned to one side.
Given that there are more than 300 known causes for headaches, your physiotherapist may determine that the neck isn’t the cause of your headache. If your symptoms indicate a different cause, they will direct you toward the proper source of treatment.
Is your neck causing you headaches?
What is a Muscle Knot?
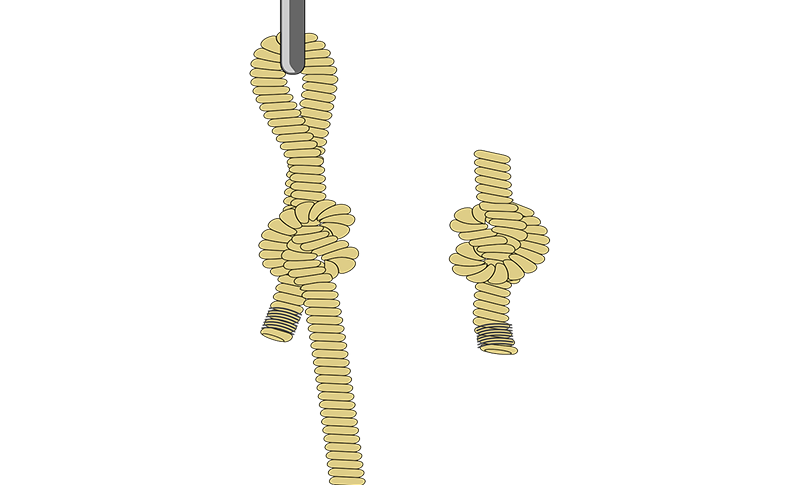
During the centuries when tall ships adorned with sails dominated the seas, any skilled sailor knew how to tie dozens of knots with intriguing names such as the anchor bend, the bowline and the half-hitch.
The knots we get in our muscles aren’t nearly so exotic or desirable; they’re painful. In addition, they’re not actually knots. So, what are they?
The Knot That’s Not
We have approximately 3-400 pairs of muscles in our bodies; as one muscle pulls in a certain direction, the other pulls in the opposite direction. Given all the work done by these muscle pairs, it shouldn’t be surprising to learn that when we work muscles hard, we may create an imbalance within the pairings. There isn’t enough distance between the muscle fibres, so the muscles can no longer glide freely and get stuck together.
This tight, painful spot that we call a muscle knot can be referred to as an adhesion – fibres sticking to each other – or a myofascial trigger point (MTP). Trigger points may only hurt when you put pressure on them or they can regularly send pain signals along your neural pathway.
Tying Those Knots or How do Knots Form?
There are three common causes for muscle knots:
- Accidents: Acute trauma to your body, such as a fall or a sports injury can strain your muscles and joints.
- Postural stress: Regularly carrying heavy objects (e.g., purses) on one shoulder, sitting too long with poor posture, sitting without support – bleachers, anyone? – or lifting heavy objects improperly.
- Overstimulation: Strenuous sporting pursuits or exercise; lifting weights.
Preventing Muscle Knots
Now that you understand a bit about the causes and the mechanics of muscle knots, you’d undoubtedly prefer to avoid them! There are steps you can take to prevent a muscle knot from developing:
- Hydration and Diet: Drink plenty of water and maintain a healthy diet. Water helps to lubricate your muscles, while caffeinated drinks, alcohol and fast foods loaded with salt help dehydrate you. Ensure that you get enough of foods that contain B vitamins, potassium and calcium, such as bananas and yogurt. If you are mindful of what you put into your body and eat and drink healthily, you are less likely to get injured.
- Lifestyle: Lack of sleep and ongoing stress makes you more vulnerable to injury. Get proper rest and don’t abuse your body. Even a short period of daily meditation or yoga can be useful for relaxation.
- Massage: It’s not just for spa days – think of professional athletes. Massage therapy is a useful tool for keeping muscles oxygenated, flexible and healthy.
- Regular Breaks: Many of us today spend our lives seated at a desk and tied to our computers. Our bodies are designed to move, and it’s unhealthy for them to remain in one position for too long. At work or at home, get up each hour and walk around a bit – fill up your water bottle, for example. While sitting at your desk, stretch your neck, uncross your legs and straighten your shoulders. Movement is good.
- Exercise Regularly: As noted above, our bodies are designed for motion. Build regular exercise into your weekly schedule so that you remain flexible and strong. A physiotherapist can assist you in determining which exercises are best for your lifestyle and physical strengths and abilities.
- Stretch: When you finish exercising and your muscles are warm, do a series of stretches to help them remain flexible.
How to Get Rid of a Muscle Knot

As much as we’d all love to avoid muscle knots altogether, they may occur. When you feel a knot and experience pain, your body is sending a signal that it needs help. Consider these possibilities to get rid of a muscle knot:
- Rest: It’s time to take a break from whatever is causing the pain, whether it’s sitting at your computer or lifting weights at the gym. Give your body some time to heal.
- Massage: While it’s great for prevention, massage therapy is also very useful as a treatment for knots. A registered massage therapist can break up your adhesions, relieve muscle pain and suggest appropriate self-care that may include foam rollers or other tools.
- Physiotherapy: If you have been bothered by pain for a while, a physiotherapist will help identify the underlying causes and will provide relief with the most appropriate techniques.
- Stretch: Gentle range-of-motion activities are usually helpful, but it is best to discuss your proposed routine with a physiotherapist, massage therapist or athletic trainer before embarking on it. Be sure that your movements are pain free.
Muscle knots are NOT insurmountable. With the proper attention, you should be able to resume your usual activities and prevent them from recurring regularly.
Bothered by muscle knots?
What are Shin Splints?
What do runners, ballet dancers and military recruits have in common? One trait they all share is a susceptibility to shin splints.
What are shin splints? A shin splint is actually an inflammation of the tendons, muscles and bones surrounding your tibia, or shin bone. Generally, the pain occurs on the inside edge of your shin bone where your muscles attach to the bone. While any vigorous sporting activity can lead to shin splints, most people associate them with running.
Shin Splits Causes
Shin splints are caused when the leg’s muscles and bone tissue are overworked by repetitive physical activity. There are a number of physical reasons that can turn overwork into inflammation:
- Excessive pronation of the foot;
- Increase in strain on a muscle;
- Overstriding;
- Local fatigue of the surrounding structures, decreasing their ability to absorb shock and transferring it to the shin bone;
- Inflexible calf muscles, lessening ankle flexibility;
- Increasing intensity in training.
People who have flat feet or unusually rigid arches are susceptible to shin splints. In addition, running in worn-out shoes can bring on this unwanted inflammation.
Discuss your symptoms with your doctor. He or she may want to conduct some tests to rule out other shin problems, such as stress fractures and tendinitis.
Shin Splits Treatment

Unfortunately, the treatment for shin splint requires rest from the activity that caused the inflammation – and that means no running for a while. Recovery can take three to six months.
For anyone working toward a goal, it can be frustrating, but you can substitute other aerobic activity such as swimming or using a stationary bike, to maintain your fitness while you recover. A physiotherapist can help prescribe a course of exercises that will keep you in shape without aggravating your injury.
You shouldn’t return to the activity that caused your shin splint until you are pain free for two weeks.
In the meantime, you should find these aids helpful in treating shin splints:
- Flexibility exercises: Your physiotherapist can assist you in choosing exercises to stretch your lower legs and ease some of the pain.
- Range of motion exercises: By exercising your ankles, knees, feet and hips, you can relieve pain, reduce inflammation and improve circulation, which aids healing. Ask your physiotherapist to suggest a course of exercise.
- Ice: Apply ice packs to your shins for 20 minutes at a time a few times a day.
- Compression: If you have swelling, a compression bandage may help keep it under control.
- NSAIDs: Non-steroidal anti-inflammatory drugs such as ibuprofen or Aspirin help reduce pain.
How to Prevent Shin Splints

In addition to the discomfort they cause, shin splints put a cramp on your training schedule. If you’re preparing for a big race, there’s nothing more frustrating than delays or obstacles that could keep you from meeting your goal. With that in mind, here are some helpful hints on how to prevent shin splints:
- Slow and steady. As you train, build up to longer distances gradually. Don’t expect to run five kilometres one week and be ready to do 10 the next.
- Mix it up. Don’t make running your only activity, given the strain it puts on your joints. Combine it with other activities, such as swimming, cycling or rowing, that give you the same cardiovascular boost without the joint stress.
- Short and sweet. A short stride length is better for your body and helps prevent shin splint. It also helps you increase speed, since quicker leg turnover leads to speed. Two benefits for the price of one!
- Make it the middle. Landing flat on the middle of your foot prevents stress and injury. If you run on your toes, your calf muscles may become strained, while striking the ground heel first stretches your shin muscles.
- Shoe cues. Give your feet the extra support they need by selecting neutral shoes or those that are designed for stability or motion control. Ask your physiotherapist for a gait analysis. If you are striking with your heel or overpronating (turning your foot outward), orthotics in your shoes may help keep you aligned properly by providing arch support. It’s an inexpensive way to keep other conditions, such as plantar fasciitis, at bay, too. In addition, make sure to replace your shoes every 500 kilometres. Worn out shoes are a major cause of shin splints, since the wear and tear erodes their support.
Prevent shin splints, but if you can’t avoid them, follow the proper course of treatment so you don’t do yourself permanent harm.
Are Shin Splints causing you discomfort?
Restless Legs Syndrome

People who work at desk jobs try to remind themselves to get up regularly and stretch, since research has shown it is better for their general health. Those suffering from Restless Legs Syndrome, however, wish they had the choice of sitting still for as long as they wished, rather than being compelled to move.
What is Restless Leg Syndrome?
Restless Leg Syndrome (RLS) is a disorder that causes an uncontrollable urge to move your legs, generally because of discomfort. Between five and 15 per cent of Canadians suffer from RLS and describe the discomfort as a pins and needles sensation under the skin, tingling, crawling or prickling.
It is also called Willis-Ekbom Disease after two physicians, centuries apart, who described the disorder: Sir Thomas Willis, a 17th-century British physician, and Karl-Axel Ekbom, a Swedish physician writing in the 1940s.
Restless Legs Syndrome can begin at any time of life and usually worsens with age. It generally makes itself felt in the evenings and can interfere with sleep. About 80 per cent of people who suffer from RLS experience a related condition, periodic limb movements, twitches and kicks that happen at while you sleep.

Movement provides temporary relief to RLS sufferers, so travel can be difficult, because sitting in a confined space for long periods of time is uncomfortable.
What Causes Restless Leg Syndrome?
Although researchers are still exploring the cause for RLS, it may result from an imbalance of the chemical, dopamine, in the brain, because its messages help control muscle movement.
Often, Restless Leg Syndrome is hereditary, especially cases that begin before age 50. It may appear during pregnancy, especially in the last trimester, but RLS usually disappears after delivery.
Low levels of iron may bring on RLS, but it usually disappears with treatment. It is also often associated with diabetes and Parkinson’s disease.
Diagnosing the Disease
There is no test to diagnose RLS. The Mayo Clinic notes that a diagnosis is based on the following criteria, established by the International Restless Legs Syndrome Study Group:
- You have an often irresistible urge to move your legs, usually accompanied by uncomfortable sensations typically described as crawling, creeping, cramping, tingling or pulling.
- Your symptoms worsen during periods of inactivity, such as sitting or lying down.
- Your symptoms are partially or temporarily relieved by activity, such as walking or stretching.
- Your symptoms are worse at night.
- Your symptoms can't be explained solely by another medical or behavioral condition.
Your physician may order other tests, such as a blood test to check iron levels or a test for nerve damage, in order to rule out other potential causes for your discomfort. You may also undergo a sleep study to determine whether you are afflicted by periodic limb movements.
Restless Leg Syndrome Treatment

You may be able to control Restless Leg Syndrome with lifestyle changes. Try the following suggestions for relief of symptoms:
- Get regular exercise. Your physiotherapist can devise an exercise therapy that will help alleviate symptoms. Avoid working out too late in the day, however, or the symptoms may intensify.
- Warm and cozy. Soak in a warm bath and massage your legs to relax the muscles. A physiotherapist can offer a massage that provides relief.
- Cut the coffee. Sometimes, avoiding caffeine alleviates symptoms, so try staying away from chocolate, coffee, tea and soft drinks for a few weeks and see if there is any improvement.
- Say om. Try relaxation techniques such as yoga or meditation. Stress aggravates RLS, so the more relaxed you are, the better.
- Sleep smartly. Fatigue worsens RLS. Develop good sleep habits. Make sure your bedroom is cool, quiet and dark. Go to bed and arise at the same time daily, whether or not it is a workday. These routines should allow for good sleep.
If non-medical remedies don’t make a difference in your discomfort, your physician may recommend medication. However, there is no perfect solution, since each of the available medications comes with its own caveats and/or side effects, including increased drowsiness and susceptibility to falling down.
RLS treatment is highly individual – there is no “one size fits all.” With the help of medical professionals, including physicians and physiotherapists, you should be able to create a relief program that works best for you.
[divider style="empty" margin_top="40px" margin_bottom="0px"]
Experiencing symptoms of Restless Legs Syndrome?
Our experienced physiotherapists are here to help you.
[button size="large" color="orange" link="https://southvanphysio.janeapp.com/"]Book Appointment Now[/button]
[divider style="empty" margin_top="60px" margin_bottom="0px"]
How to Exercise Without Injuries
It may be winter and cold or snowy, but exercise still figures prominently in many people’s schedules. If you’ve just started an exercise regimen or tend to just do what you’ve always done without giving it much thought, it’s time to pay closer attention to how you prepare for exercise and how you execute.
The older you get, the easier it is to get injured by doing too much, not being warmed up or making an awkward movement, so why not get into the good habits that help prevent exercise injuries?
Hydration
You wouldn’t start your car without gasoline, so don’t start your body without proper hydration. Water lubricates your system and helps prevent injuries while working out. Ideally, start drinking water 20 minutes before your workout to allow it time to percolate through your system. Drink throughout your activities and afterward to replace fluids lost through sweating.
Nutrition
Exercise requires energy, and you want to make sure your body is ready to take on the challenges you impose on it. It needs access to glycogen for muscles to work properly; otherwise, they are subject to tears that may take time to heal. Don’t put yourself out of action unnecessarily.
Eating carbohydrates prior to working out is helpful in improving performance and may allow you to exercise for a longer period or at a higher intensity. Consuming protein after a workout helps to repair damage done to muscle fibres.
Circulation and Muscles

Start any workout, including a run, with a bit of light cardiovascular movement to get your blood moving through your system easily and to loosen your muscles. Jump rope, jog in place or ride an exercise bike for 5 or 10 minutes.
Flexibility
Give your flexibility a boost by doing some stretches after your warm-up. They will help your body handle the stress of exercise without injury.
Best Before Date
Overextending yourself isn’t the best way to demonstrate just how youthful, macho or cool you are. Be realistic as you assess your capabilities and plan an exercise program. Don’t simply assume you can do whatever routine it was you last tried, since that may have actually been years ago. It’s easy to do too much exercise for too long with too much intensity, resulting in injury. So, be realistic and aware.
Sex Matters
We’re talking about gender here. Men and women have different physical susceptibilities that may make certain injuries more likely. It doesn’t mean that men or women should refrain from specific activities; it’s just a reminder to be aware of the dangers before jumping into the fray.

Generally speaking, men are better at activities that use a rigid plane of motion: Nautilus machines and push-ups, for example. Women usually excel at activities that use multiple or diagonal planes of motion: yoga, Pilates, cycling and stair climbers, for instance.
Variety is the Spice of Life
Triathlons have gained in popularity for a good reason: they require athletes to cross-train, using different muscles for the swimming, biking and running portions of the competition, which helps prevent overuse and injury. Take a leaf from their workout notebooks and vary your routine. If you focus on cardio one day, try strength the following day and put your energies into stretching the next.
Relax
Rest should also be part of any exercise routine. Remember, your body, like any machine, can break down if not maintained properly. Take at least one day a week off from exercising to allow your body to heal itself. In addition, if you’re feeling tired or sore, there’s no shame in skipping a workout. It’s more likely that you’ll be injured during exercise when you’re exhausted and not using proper form. A hot bath with Epsom salts works wonders for sore muscles.
Chill Out
A cool down is especially important if you are engaged in a high-intensity exercise that increases your heart rate and puts a heavy strain on muscles. It allows you to reduce your heart rate gradually and resume normal breathing. It also prevents muscle soreness.
So, get moving – but keep all of these suggestions in mind so you can continue moving injury free!
Experiencing PAIN from your exercise routine?
Does Back Pain Go Away on its Own?
Your back is probably one part of your body that doesn’t require much thought – unless it’s hurting. Unfortunately, according to Statistics Canada, four out of five Canadians, or 80 per cent, will experience back pain during their lifetimes.
In all likelihood, back pain will strike between the ages of 30 and 50. Even more disconcerting, in 80 to 90 per cent of cases, it won’t be possible to identify the cause of this pain and the pain is likely to recur.
Standard Back Pain
The spine, muscles and ligaments are the building blocks of your back. It actually should come as no surprise that back pain is nearly universal; after all, the spine is a complex structure, itself comprising both cartilage disks and bone, that allows the body to accomplish a variety of disparate tasks, such as walking, bending and twisting.
Injury to any of these components can result in back pain. Usually, the pain is acute and will eventually subside. However, some people suffer long-term or chronic pain and require ongoing treatment and/or exercise.
The following conditions are common causes for back injury and the resulting pain:
- Obesity
- Improper warm-up before exercise
- Sedentary lifestyle
- Deformities
- Degenerative diseases, such as osteoarthritis
- Poor posture
- Weak abdominal muscles

If you assume that your back pain will simply go away, you may cause additional damage. Your first reaction may be bed rest, but that can lead to stiffness and make movement more challenging.
How to Treat Back Pain
When you first experience back pain, it’s important to treat yourself gently. Most back pain is related to muscle strain and will ease within a few days. Take these initial measures to aid recovery:
- Easy does it. Ease up on your activities and refrain from putting extra pressure on your back.
- Chill out, then heat things up. Ice your back for the first 48 hours after the injury makes itself known. The cold initially slows swelling and inflammation while numbing the pain. After 48 hours, however, it’s important to get blood flowing into the area to promote healing and relax spasms.
- Over-the-counter help. Unless you are taking prescription drugs that would interfere, use an over-the-counter medication to relieve pain and promote healing. Non-steroidal anti-inflammatory (NSAID) drugs are effective for pain relief and reduction of inflammation, but they are only intended for short-term use. Don’t continue to rely on them for more than a week. If NSAIDs aren’t permitted, try acetaminophen, although be aware of its potential side effects.
- Rub-a-dub-dub. Take advantage of a gentle massage by your partner to help stretch tight ligaments and muscles, which, in turn, may offer some relief.
- Keep moving. Restrict your activities, but don’t stop moving altogether. Motion is more effective than bed rest in treating basic back pain.

If your pain persists, it’s time to check in with a healthcare professional. In fact, it may be worth considering preventive measures before back pain strikes unexpectedly. Your family physician may refer you to a physiotherapist who can provide a course of rehabilitation or preventive exercises.
Good Back Health
Meanwhile, lend yourself a helping hand by following these tips to good back health as you move through the day:
Sitting
- Don’t stay seated for more than 10-15 minutes t a time. Get up and stretch or walk around.
- Sit in a high back chair with arm supports to prevent you from rounding your spine.
- To rise, move to the front of your chair and straighten your legs, rather than bending at the waist.
- Don’t lean over your work or hunch your back. Adjust your workstation accordingly.
Standing
- Stand properly with your shoulders straight, chest forward, head up and hips tucked in. Balance your weight evenly on both feet.
- Avoid standing in the same position for too long.
Even if you experience back pain, it can be addressed and managed. Don’t ignore it.
Experiencing BACK PAIN?
How to Maintain Good Posture as You Age
Many of you have childhood memories of your parents saying, “Stand up straight” and “Don’t slouch.” At the time, it seemed like just one more rule or annoyance that made you roll our eyes. Little did you know that their admonitions were not empty instructions, but a prescription for better health as you age.
What is Proper Posture?
It varies, depending on whether you are sitting or standing. When sitting at a desk, your knees should be level with your hips and your feet should be flat on the floor. Crossing your legs can impair circulation. If you are standing, try to stand with weight distributed equally on both legs. Your shoulders should be back and your chest slightly out with the ears positioned over the shoulders.
Why is Good Posture so Important?
It can keep you looking younger and staying healthier as you age. Proper posture helps prevent a myriad of health issues, including:
- Decreased range of motion. Your muscles and ligaments can tighten or stretch if you regularly sit in a slumped position. Once this happens, these muscles and ligaments don’t function properly.
- Decreased lung capacity. Good posture allows the appropriate amount of air to flow through your lungs. Otherwise, your chest cavity may decrease in size and prevent your lungs from functioning properly.
- Low back pain. A major consequence of poor posture.
- Increased discomfort. Poor posture can lead to headaches and pain in your shoulders, arms and hands.
- Jaw pain. If your head is thrust forward, it can result in temporomandibular joint disease, once considered solely a dental problem.
- Spine misalignment and rounding. Poor posture can result in a spine that is out of position and may lead to interference in nerve function. Osteoporosis can cause compression or destruction of vertebrae.
How to Maintain Good Posture?
Now that you have incentive to stand tall, how can you make sure you maintain good posture? It’s not as difficult as you may fear; it just requires a bit of time and effort.

Try these approaches:
- Stay limber. If you spend most of your day sitting at a desk or in front of a computer, it’s important to maintain a good range of motion. Get up for a few minutes each hour and stretch your arms overhead with fingers interlaced or walk around a bit to keep the body moving.
- Stay flexible. Each morning, lie on the floor and make snow angels for a few minutes to stretch your muscles. You can challenge yourself by placing a foam roller or a rolled up towel under your spine for an extra stretch. Go slowly and stop if you feel anything other than mild discomfort.
- Sit up straight. Good posture while sitting is a habit worth cultivating. It requires strong core muscles, so consider some strengthening exercises, yoga or Pilates; the abdomen is the heart of good posture and helps improve everything from urinary incontinence to sex.
- Correct your computer. If you work at a computer, be sure that your eyes are level with the screen and that your arms and wrists are straight and parallel to the floor.
- Strengthen your spine. Women have weakening around the spine after menopause so it’s crucial to keep the surrounding muscles strong. Strong spine and trunk muscles are especially important when you need to stand for long periods of time. Inquire at your gym about exercises or machines that strengthen the back extensors, neck flexors, pelvic muscles, and side muscles.
- Add some weight. Build some weight-bearing exercises into your routine. Osteoporosis, the disease that thins your bones, can cause vertical compression fractures that make us shorter as we age and even lead to dowager’s hump. Weight-bearing exercises help prevent a loss of bone density, so consider lifting weights, walking or climbing stairs to keep you tall and strong.
- Check your calcium intake. Calcium is important for building strong bones. Women between the ages of 19 and 50 need 1,000 milligrams daily; after 50, the recommended dose increases to 1,200 mg. Usually, a healthy diet provides the necessary amount, but there are supplements available, although they may make you more susceptible to other health problems.
Monitoring your Posture
It’s never too early or too late in life to improve posture. Before you undertake an exercise regimen, document your current posture to establish a baseline for future comparison.

Put on your exercise gear or wear comfortable clothes and ask someone to take full-length photos of you from the front, the side and the back. If you do this once a year, you can see if changes are taking place and work to correct them. In addition, monitor your posture as you walk past mirrors to ensure that you are standing tall.
Remember, although everyone ages, numerical age can also be a state of mind – and body. If you have good posture, you’ll look younger and feel younger, too.
Experiencing PAIN from POOR POSTURE?
How to Avoid Weekend Warrior Injuries
We’ve all been in this position at some point in our lives: the Olympics are underway and we’re oohing and aahing over the incredible feats being performed by the athletes, so we’re inspired with a desire to emulate them. Soon, we’re lacing up our running shoes and setting out on the roads or diving into the pool, even though we may not have participated in either of those sports in ages.
Afterward, of course, our bodies let us know how foolish we have been. If we’re lucky, we may get away with sore muscles; if things go badly, we may suffer a sports injury that needs treatment and healing.
The Most Common Weekend Warrior Injuries
Of course, it’s not only during the Olympics that these unfortunate injuries occur. As we age, those of us who participate in a sport on the weekend, but are sedentary throughout the week, are ripe for sports injuries.

Weekend warriors, as they’re commonly called, don’t use their muscles regularly, so it’s no surprise their bodies aren’t prepared for the strain put upon them when it’s time for pickup hockey or the weekly softball outing.
Among the common injuries from weekly outings are:
- Ligament sprains
- Stress fractures
- Muscle strains
- Tendinitis
- Shin splints
- Runner’s knee
- Tennis elbow
How to Prevent Weekend Warrior Injuries
Most weekend warrior injuries are preventable. There’s no need to put your body at risk of injury if you approach physical activity properly.

Here are some tips to prevent injury while you enjoy your athletic pursuits:
- Challenge your body: Professional athletes train regularly to stay at the top of their games, so why should you expect to jump onto the ice one night each week and instantly perform like Sidney Crosby? Nor can you ever recapture your glory days as a high school basketball star – youth has its advantages. However, there is no reason you can’t perform well as long as you prepare. Try to challenge your body at least twice a week by using the muscles you’ll be using in the game or the competition so they are ready for the workload you will expect them to undertake.
- Bet on balance: Once you’ve decided to exercise more than once a week, employ some balance in the activities you choose. Include cardiovascular activity, stretching and weight training in your routine. Cross-training can prevent injuries that result from overuse: relying on the same group of muscles and tendons regularly.
- Slow and steady: As much as you’d like to run a marathon the week after you’ve started jogging, it’s unrealistic and dangerous. Begin with a level of intensity that is manageable and increase it by 10 per cent weekly, allowing your body to become accustomed to the new level of activity.
Stretching, Hydration and Equipment
Stretching is important for everyone over the age of 30. Muscles get tight, especially leg muscles. If they are overused, the body will compensate by relying on other areas, such as the lower back.

- Get warm: Stretching before your activity may relax key muscles, shutting them down so that they are susceptible to strains; they will be less receptive to dynamic movements. Instead, consider an active warm-up. Hockey players take their warm-up skate before a game, and you should also prepare your body for activity with movements that increase the blood flow to soft tissues while activating muscles. Examples of active warm-up moves include high knees, shuffling, throwing and jogging.
- Hello, hydration: People generally don’t drink enough fluids during the day, so it’s likely that you’ll begin your athletic pursuit at a disadvantage. Research has shown that even a five per cent loss of bodily water content can have a major impact on agility, reaction time and speed. Don’t wait until you are thirsty to drink – by the time you notice your thirst, you’re already dehydrated. Instead, get in the habit of drinking water or other replenishing fluids at regular intervals throughout your day. Soon, it will seem like a no brainer.
- Equip yourself: Ensure that you have the proper equipment for the sport you are undertaking, and make sure the equipment is in good shape so that it doesn’t contribute to possible injury. Shoes, for instance, break down and can’t offer the necessary foot stability. They can also lead to foot injuries if your wear pattern results in a compromised foot position. The rule of thumb – or foot, in this case – is to get new running shoes after about 800 kilometres (500 miles) of use.
How to Deal with a Weekend Warrior Injury
If you have ventured onto the playing field before reading this article, you may already have first-hand knowledge of weekend warrior injuries.

If you do suffer an injury while playing sports, follow the RICE method:
- Rest the injured area to allow for healing.
- Ice the injury on and off for 10 to 15 minute periods during the day to keep swelling down and alleviate pain.
- Apply compression to the affected area.
- Elevate the injured area above heart level to prevent or decrease swelling.
If the RICE method doesn’t yield results or you are still in pain, don’t shrug off the injury.
Physiotherapists can do movement assessments, provide treatment and design appropriate home exercise programs to assist your healing. There’s no need to suffer endlessly as a result of being a weekend warrior!
Suffering from a weekend warrior INJURY?
Distracted Driving in BC: What You Need to Know
All licensed drivers have been taught the rules for driving safely, including no tailgating, signal before turning and not mixing drinking alcohol and driving. One rule that British Columbia drivers find all too easy to break, however, is avoiding distracted driving.
What is Distracted Driving?
Distracted driving refers to driving while participating in activities that impact the driver’s ability to focus on the road. It can result from visual distractions inside or outside the vehicle or from cognitive distractions such as conversations and using electronic devices.
Distracted Driving Statistics
Although you may pride yourself on the ability to multi-task, distracted driving is more dangerous than you may realize. Police statistics indicate that 27 per cent of all traffic fatalities in BC are the result of distracted driving. There is an average of 81 fatalities annually as a result of distracted driving – behind only speeding, with 94 and ahead of impaired driving with 78.
In fact, most rear-end accidents that result in injury are due to distracted driving. Injuries to the upper spine and neck (e.g., whiplash) are the most common ailments resulting from rear-enders and may require a visit to your physician and a course of physiotherapy.

More Dangerous Than Drinking and Driving?
One of the most common causes of distracted driving is the use of personal electronic devices. Research has shown that when you’re simultaneously driving and talking on a cellphone you lose 50 per cent of your awareness of what is going on around you, so you’re ripe for an accident. In fact, you are five times more likely to crash if you’re talking on your cellphone.
Even though 90 per cent of B.C. drivers surveyed in 2015 by Ipsos rated texting while using a cellphone as more dangerous than drinking and driving, one in five of them – 20 per cent – admitted to texting or making a call using a hand-held device recently while driving.
Distracted Driving Laws in BC
The British Columbia government amended the Motor Vehicle Act in 2010 to include hand-held devices. According to the Insurance Corporation of British Columbia (ICBC), section 214.2 of the Act tells motorists that “a driver cannot operate a hand-held electronic device (including hand-held cellphones, smart phones, tablets and other electronic hand-held devices such as music players, GPS Navigation Systems, etc.). Also, a driver cannot communicate using text messages or email on any type of electronic device.
“Drivers with a regular licence are permitted to use hands-free cellphones and devices that can be operated with one touch or voice command, provided that the device is securely fixed to the vehicle or worn securely on the driver’s body.”
Anyone who is first earning a driver’s license through the province’s Graduated Licensing Program (GLP) is forbidden from using hands-free cellphones while driving.

Penalties for Distracted Driving in BC
Beginning June 1, 2016, the B.C. government increased the penalties for using a hand-held device while driving. A ticket for a first distracted driving moving violation more than doubled in cost to $368 (from $167) and adds four points to the driver’s record.
There is also an additional $175 ICBC Driver Penalty Point premium, which brings the total fine to $543, plus the points. Fines become steeper as infractions mount.
Distracted driving is also considered one of the high-risk driving infractions that lead to early intervention and driving prohibitions as part of B.C.’s Driver Improvement Program. Any driver who collects two or more violations within a 12-month period will have their driving record reviewed by the program and may be prohibited from driving for three to 12 months.
Any beginning driver who is part of the GLP will be subject to licence review after one infraction and may be prohibited from driving for one to six months, with more severe penalties for further infractions.
What’s Permitted – and What Isn’t
To avoid any of the aforementioned penalties, be aware of what is and isn’t true about distracted driving:
Red Lights Mean Stop Texting. Contrary to popular opinion, you are NOT permitted to text or use a hand-held device while stopped at a red light or in traffic. You are still behind the wheel and it is still against the law.
I’ll Just Play Music. It’s against the law to use ANY features of your hand-held device while driving. So, no checking voicemail, choosing songs or looking at a GPS.
Speakerphones Are Fine. You can use a hands-free cellphone with a Bluetooth or wired headset, but your phone must be securely attached to your body (via a belt clip or in your pocket), rather than lying loose on the seat, in your lap or in your cup holder.
Emergency Calls Are OK. You are exempt from penalties if you are calling 9-1-1 about an emergency requiring fire, police or ambulance service. However, the exemption doesn’t extend to family emergencies.
Now that you know the rules about driving distractions, stick to them. If you can’t resist the temptation to use your phone, try locking it in the trunk while driving, or pull over to the side of the road to take calls. It’s not worth your life to take your mind off your driving.
Have you been INJURED in a car accident?
Physiotherapy Exercises: Balance, Range of Motion and Strengthening
Whether you are seeing a physiotherapist for help in regaining leg strength after a hip replacement or to build up some aerobic capacity after heart surgery, your visit will have one commonality: physiotherapy exercises will be involved. After all, physiotherapy can be defined as a treatment method that focuses on the science of movement and helps people to restore, maintain and maximize their physical strength, function, motion and overall well-being. It’s all about learning to make the proper moves.
Physio Moves: The Most Common Physiotherapy Exercises Explained
Although each patient’s physiotherapy program is unique and tailored to the nature of their physical issues, there are three types of physiotherapy exercises commonly included in rehabilitation programs:
- Balance
- Range of Motion
- Strengthening
Balance Exercises
Physiotherapy can explore both static and dynamic balance. Static balance refers to control of your stationary body, while dynamic balance refers to the control you have over your body while it’s moving. Deep core stability and hip and leg muscle control are essential for good balance.
Without good static balance, you may be prone to falls and their unpleasant consequences: fractures. As people age, their bones are more fragile and hips and pelvises are more vulnerable.
When your dynamic balance is impaired, you end up with poor muscle and joint control that can lead to instability-related conditions such as back pain, sciatica, hip pain, bursitis or knee pain. Poor dynamic balance also affects your sporting pursuits, because you are not working from a stable platform.
Balance exercises work to improve both balance and proprioception, or awareness of joint position. They help you to adjust and maintain as your centre of gravity shifts. Five minutes a day of balance exercises is a good start, and your exercises should not cause symptoms or increase them.
Possible balance exercises include:
- Single Leg Balance: Stand on one leg with arms extended and attempt to maintain your balance for a minute.
- Single Leg Pillow Balance: Stand on one leg on a pillow with arms extended, maintaining your balance for a minute.
- Heel-Toe Walk: Slowly walk in a straight line, carefully placing one foot down and bringing the other foot in front, touching the heel of the front foot to the toe of the rear foot.
Range of Motion Exercises
Range of motion refers to the movement of a joint from its fully flexed position to its fully extended position. Although each joint has a normal range of motion, the amount of joint movement varies from person to person.
There are three types of range of motion exercises: passive, active-assistive and active.
- Passive range of motion exercises: As you remain still, the physiotherapist will move your limb along the joint range; it is often done if you are unable to move a limb yourself.
- Active-assistance exercises: Although the patient can move the limb, the physiotherapist helps complete the motion along the joint range or until the point that pain kicks in.
- Active exercises: The patient performs the movement without any assistance from the physiotherapist.
Here is a sample of range of motion exercises for various body parts:
- Neck: Head tilts, forward and back: Bow your head gently and try to touch your chin to your chest. Now, move your head back to the starting position. Next, tilt your head back as far as possible so you are looking at the ceiling; return your head to the starting position.
- Shoulder: Shoulder rotation: Raise your shoulders up toward your ears, as if you were shrugging. Lower them to the starting position, and relax. Pull your shoulders back. Then relax them again. Roll your shoulders forward in a smooth circle; reverse direction and roll your shoulders smoothly backward.
- Legs: Leg lifts: Lie on your back and raise your leg so that it is 15 to 31 centimetres off the floor. Hold for 30 seconds. Return to the floor. Repeat.
Strengthening Exercises
Strengthening exercises are done to ensure that your muscles have normal strength, in order to prevent future injury. In situations where your muscles have not moved for a while due to injury, strengthening is essential.
Exercises to increase muscle strength fall somewhere in type between the high repetitions and low resistance of endurance training programs and the fewer repetitions and high weight load of the programs designed to increase muscle size.
Here is a sample of strengthening exercises for core stability:
- Transverse Abdominus: This muscle is a key stabilizing muscle in the abdomen. Lie on your back and slowly draw the section of your abdomen situated below your belly button upwards and inwards away from the line of your belt and breathe normally. Keep your rib cage relaxed and not elevated. Practise holding this muscle at 20 to 30 per cent of a maximum contraction for 10 seconds; repeat 10 times.
- Plank or Prone Hold: Lie down on your stomach. Prop yourself up on your elbows and toes and hold for as long as possible.
Ideally, you should see a physiotherapist for an exercise program that is tailored to your needs. Remember, physiotherapy exercises can be preventive as well as rehabilitative.
Looking for a TAILORED exercise program?
What is Physiotherapy?
A common question for people that have never visited a physiotherapist is the very basic question of “What is Physiotherapy?”. Physiotherapy encompasses rehabilitation, injury prevention and health promotion/fitness. The profession employs a holistic approach to treatment, looking at the patient’s lifestyle and engaging them in their own treatment.
Physiotherapy Definition
Physiotherapy can be defined as a treatment method that focuses on the science of movement and helps people to restore, maintain and maximize their physical strength, function, motion and overall well-being by addressing the underlying physical issues.
How to Become a Physiotherapist - Physiotherapy Canada
The healthcare professionals who provide physiotherapy are called physiotherapist. They are highly trained, with master’s degrees in physiotherapy, and are skilled at pinpointing the root causes of an injury, as well as treating them. Often, a problem originates in a completely different part of the body than the spot where the pain is centralized.
Physiotherapy is a registered profession in Canada. The Canadian Physiotherapy Association notes that physiotherapists:
- Have met national entry-level education and practice standards;
- Have successfully passed a standardized physiotherapy competence examination; and
- Are registered with the college of physiotherapists in their province/territory.
Once they are certified and registered, physiotherapists can pursue the designation of clinical specialist. This program, run by the Canadian Physiotherapy Association, “certifies physiotherapists who have focused their careers and can demonstrate advanced clinical competence, leadership, continuing professional development and involvement in research in a specific area of practice.”
Candidates for the clinical specialist designation must have a minimum of five years of applied clinical experience and a minimum of 300 clinical contact hours per year for the past five years in the clinical specialty area.
Physiotherapists work in concert with other healthcare professionals, and physicians may recommend a course of physiotherapy after an injury, surgery (e.g., hip replacements) or such health issues as heart attacks or strokes.
Physiotherapy Treatment: What Conditions do Physiotherapists Treat?
As professionals, physiotherapists are experts at providing physiotherapy treatment for:
- Preventing injury and disability;
- Managing acute and chronic conditions;
- Improving and maintaining optimal physical performance;
- Rehabilitating injury and the effects of disease or disability;
- Educating patients to prevent re-occurrence of an injury.
Patients may be referred to or seek assistance from a physiotherapist for a variety of health issues and receive valuable assistance.
Physiotherapists offer treatments relating to the following conditions:
- Cardiorespiratory: providing support, prevention and rehabilitation for people suffering from diseases and injuries that affect the heart and lungs, such as asthma.
- Cancer, palliative care and lymphedema: treating, managing or preventing fatigue, pain, muscle and joint stiffness, and deconditioning.
- Incontinence: managing and preventing incontinence and pelvic floor dysfunction.
- Women’s health concerns: addressing health issues surrounding pregnancy, birth, post-partum care, breastfeeding, menopause, bedwetting, prolapsed, loss of bladder or bowel control.
- Musculoskeletal: preventing and treating clients with musculoskeletal conditions such as neck and back pain.
- Neurological: promoting movement and quality of life in patients who have had severe brain or spinal cord damage from trauma, or who suffer from neurological diseases such as stroke, Parkinson’s disease and multiple sclerosis.
- Orthopedic: helping patients prevent or manage acute or chronic orthopedic conditions such as arthritis and amputations.
- Pain: managing or preventing pain and its impact on function in patients.
Physiotherapy Techniques: What Techniques do Physiotherapists Use?
Physiotherapists employ a variety of techniques, depending on the nature of the injury or problem they are treating. The most common physiotherapy techniques are:
- Manual manipulation: Moving joints and soft tissue helps to improve circulation, drain fluid from the body, and relax overly tight or muscles with spasms.
- Electrical nerve stimulation: Small electrical currents delivered to affected areas helps to suppress and block pain signals to the brain.
- Acupuncture: Needles stimulate the nervous system and work to dull pain, release muscles, boost the immune system and regulate various body functions.
- Demonstration: Teaching proper movement patterns allows patients to help heal themselves.
- Functional testing: Testing a patient to assess his/her physical abilities.
- Device provision: Prescription, fabrication and application of assistive, adaptive, supportive and protective devices and equipment.
What to expect from a visit?
Each session with a physiotherapist is unique, because it depends on the client’s health issues and needs. However, a visit to a physiotherapist generally includes:
- Learning about the patient’s medical history;
- Assessing and diagnosing the patient’s condition and needs;
- Helping the patient set and reach physical goals;
- Creating a treatment plan that accounts for patient’s health, lifestyle and activities;
- Prescribing a course of exercises and necessary devices.
If you are experiencing issues with movement or function or are just seeking to optimize your health, why not check out a trusted resource like a professional physiotherapist.
Having issues with your MOVEMENT?
What is Shoulder Impingement Syndrome?
How can you shoulder your burdens properly if you are suffering from shoulder impingement syndrome?!
All kidding aside, if your shoulder hurts when you try to reach behind your back or retrieve an object from a high shelf, you should see your physician. Since the shoulder comprises a number of bones, muscles and tendons that allow for a range of motion in your arm, it is vulnerable to a variety of complaints.
Shoulder impingement syndrome, also known colloquially as swimmer’s syndrome or thrower’s syndrome, is the irritation of the tendons in your shoulder caused by rubbing against bone. To understand how it happens, let’s first discuss how the shoulder operates.

A Bit of Anatomy and Physiology
Three major bones comprise your shoulder: your upper arm bone (the humerus), the collarbone (the clavicle) and the shoulder blade, or scapula. The latter two bones create a socket for the humerus, which is protected at the top by muscles and tendons that hold your arm in place. These are called your rotator cuff.
A lubricating sac, or bursa, forms a protective covering between the rotator cuff and the upper bones of the shoulder. The lubrication allows the rotator cuff tendons to glide freely through the bridge created by these upper bones.
Shoulder impingement syndrome results when bone rubs on the bursa and tendons and irritates them. Eventually, it can lead to inflammation of the rotator cuff tendons (tendinitis) and bursa (bursitis).
Treatment for shoulder impingement syndrome is important; otherwise, the tendons may start to thin out and tear. We’ve all heard stories about professional baseball players needing to rehabilitate a torn rotator cuff.
Impingement Syndrome Shoulder – Who Is Susceptible?
Rotator cuff pain, including impingement syndrome shoulder, is common among both young athletes and middle-aged adults. Athletes who repetitively raise their arms overhead, such as swimmers, tennis players and baseball players are particularly susceptible. Among adults, those who repeatedly lift things overhead, such as construction workers or painters, are also at risk.

Types of Shoulder Impingement
Shoulder impingement is classified as either internal or external.
External impingement refers to a structural abnormality or interference with the proper operation of the rotator cuff. Primary impingement is generally due to the abnormally shaped arch in the shoulder bones or to bone spurs that come with degeneration of the bone. Secondary impingement usually results from poor shoulder blade stabilization that changes the position of the arch and causes rubbing; it can also be a consequence of tendons weakened from overuse.
Internal impingement generally occurs in athletes whose sports focus on throwing, such as javelin or baseball. The underside of the rotator cuff tendons rubs against a different bone (glenoid labrum) to cause pain at both the back and front of the shoulder.
Ouch, It Hurts!
Initially, symptoms from shoulder impingement syndrome can be mild and sufferers may not immediately seek treatment. Athletes may have pain when throwing or serving a tennis ball, while others may experience sudden pain when they reach or lift. Pain may radiate from the front of the shoulder to the side of the arm. There may be minor pain both during activity and while at rest.
As the impingement becomes more severe, there will be pain at night and loss of strength and motion. Activities, such as zipping a zipper, that require an arm to reach behind the back will become difficult. When this happens, it’s definitely time to seek medical attention.

Diagnosis of Shoulder Impingement Syndrome
When your doctor examines you, he or she will test your shoulder for range of motion. You may also be required to undergo an MRI test, since they are useful for soft tissue injuries and may show the inflammation. An X-ray may be taken if bone spurs are the suspected cause of the impingement.
Shoulder Impingement Syndrome Treatment
Shoulder impingement syndrome treatment will generally begin with non-surgical options, including rest from activities that are suspected causes; non-steroidal anti-inflammatory medicine to reduce swelling and pain; and physiotherapy.
Your physiotherapist will work with you towards restoring the normal range of motion. Shoulder impingement syndrome exercises may include stretching exercises to relieve pain and improve motion. Once the pain in your shoulder begins to subside, your physiotherapist can work with you on strengthening your rotator cuff muscles so the shoulder impingement syndrome doesn’t recur.
If this course of shoulder impingement syndrome treatment doesn’t alleviate your pain, you make receive a shot of the steroid cortisone, since it is a powerful anti-inflammatory.
When all else fails, surgery may be necessary to create more space in your body for the rotator cuff. Generally, the surgeon will remove the inflamed portion of your bursa and may also remove a piece of the arch bone that rubs against the rotator cuff.
If surgery is required, you will probably need to wear a sling for a period of time to support the shoulder as it heals. Physiotherapy will then assist you in regaining motion and strength.
Remember, don’t ignore pain in your shoulder, because your body is signalling that something is wrong.
Suffering from SHOULDER PAIN?
What is a Soft Tissue Injury?
Coping with a soft tissue injury can be hard, depending on its severity. For active people, it can mean being out of commission for six weeks or more. Without giving rest and recovery their proper due, however, soft tissue injuries can easily recur.
Soft Tissues and Soft Tissue Injury Explained
The term soft tissues refers to muscles, ligaments, tendons and fascia, the connective tissues that bind the body together. Injuries to these tissues are generally tears, pulls or contusions and may occur as the result of a one-time incident, such as a misstep; though repeated use over time, such a work-related injury; or through overuse of fatigued muscles, such as running too soon after a marathon.
Soft tissue injuries are categorized into three grades:
Grade 1: Mild. Usually involves no more than 10 per cent of the muscle or ligament and will heal in a week or two.
Grade 2: Moderate. Involves 10 to 90 per cent of the tissue structure. Healing takes several weeks.
Grade 3: Severe. Severe tears; complete rupture of muscle or ligament. Will require physiotherapy over time to rehabilitate.
Common Soft Tissue Injuries
Some common soft tissue injuries include:
- Back strains and sprains
- Ankle strains and sprains
- Torn ligaments in the knees, shoulders and ankles
- Plantar fasciitis
- Carpal tunnel syndrome
- Tennis elbow
- Bursitis
- Tendinitis

How Bad Is It?
If any of these conditions apply to your injury, you should have it assessed by a physician:
- You are unable to put any weight on the injured area
- The injured area now has an unusual shape or looks deformed
- You heard a pop or crack when the injury occurred
- Any of the surrounding bones feel painful
- You feel numbness or pins and needles around the injury or anywhere else
Soft Tissue Injury Treatment: First Steps to Recovery
If you injure yourself, you want to contain the damage and start the healing process as soon as possible. During this acute phase of the soft tissue injury, while the swelling, bleeding and pain are at their height, you want to protect yourself from further injury.

The first step of your soft tissue injury treatment is to stop the activity you were doing when the soft tissue injury occurred and following the RICE method: rest, ice, compression, and elevation.
Rest: Take any load off the injured body structure. Avoid all activities that cause pain and allow yourself time to recover.
Ice: Reduce the pain and swelling by applying ice to the injured area in the form of cubes or crushed ice wrapped in a towel; frozen peas – they mould nicely to the injured body part; or a sports ice pack. Ice for 20 minutes every two to three hours while you’re awake.
Compression: Wrap with a bandage that doesn’t obstruct blood flow or cause additional pain. This helps keep the area stable.
Elevation: To reduce pain and swelling, raise the injured area above the level of your heart, supporting it with pillows or a sling, as needed.
During the acute phase of injury, it’s also important to avoid HARM: heat, alcohol, running and massage. You don’t want to increase the blood flow too soon – it will only increase damage. This phase, during which the soft tissue injury settles, generally lasts a day or two.
Moving Toward Full Recovery
Once your soft tissue injury has stabilized, your body will enter the sub-acute phase, repairing itself by laying down new tissue that strengthens over time, reducing the need to protect the injury. During this phase, a physiotherapist will usually assess your soft tissue injury and oversee your soft tissue injury treatment.

You will likely be given a mix of passive treatments, hands-on mobilization, rehabilitative exercises and support. Rehabilitation time depends on the severity of the injury, your own physical health and your age.
Passive treatments stimulate the injured area to promote the healing response by increasing energy to the site using electrical stimulation, ultrasound, magnetic field therapy or laser stimulation. Your physiotherapist may also manipulate your joints and will assign you exercises designed to help return your body to normal functioning. You may need to wear a brace or strap your injury to provide it with additional support as it heals.
Remodelling Yourself – Soft Tissue Injury Healing Time
Six weeks after injury, your body enters what is often termed the remodeling phase. Your new tissue is fairly strong, but it hasn’t stop regenerating. If the tissue isn’t strong enough to handle the level of activity you require, it will continue to stimulate the growth of more tissue so that your body can support you properly.
Remember: your treatment and soft tissue injury healing time depends on your injury, your age and your body. Don’t measure your progress against anyone else’s because everyone’s body is unique. Follow the advice of your physician and your physiotherapist and your body should return to its recognizable self.
Think you have a SOFT TISSUE INJURY?
What is a Frozen Shoulder?
It’s understandable if the thought of a frozen shoulder sends a chill down your spine, because it is a condition that equates to loss of mobility, something no one wants to experience. Frozen shoulder, also known as adhesive capsulitis, is a condition resulting when there is injury and inflammation in the soft tissues surrounding the shoulder.
The shoulder is a ball and socket joint, and the head of the upper arm bone, the humerus, fits into a cavity created by the shoulder bone, the scapula. The inflammation in this capsule makes movement more difficult and painful. The joint may also lose some of the synovial fluid that lubricates it.
However, reduced movement causes capsule to thicken and contract, leaving less room for the shoulder joint to move around, so it is actually a vicious cycle: the shoulder is painful, so you move it less often, but the less you move it, the more likely the capsule is to contract. In advanced cases, scar tissue can form between the upper arm bone and the capsule.
What is the main cause of Frozen Shoulder?
Frozen shoulder often occurs when a person doesn’t undergo therapy after an injury or a bout of tendinitis. It can also happen following a period of enforced immobility, such as being bedridden after a stroke or heart attack, or occur following a fall or an automobile accident.
Adults over 40 are most susceptible to frozen shoulder, and more women experience it than men. Diabetics are also susceptible. The condition may appear without any obvious injury or inflammation.
Frozen Shoulder Stages: A Three-Stage Concern
The development and healing of frozen shoulder is generally divided into three stages: the freezing stage, the frozen stage and the thawing/healing stage.
During the freezing stage, the inflammation has occurred. The shoulder stiffens and hurts and movement becomes challenging. The pain is generally worse at night. There are five symptoms generally associated with inflammation: pain, swelling, heat, redness and loss of function.
Once the shoulder is frozen, the inflammation begins to subside, because the shoulder capsule has thickened and reduced range of motion.
“Thawing” a frozen shoulder refers to eradicating the conditions that caused it, allowing for movement and disappearance of pain. Once inflammation has subsided, it is possible to move the shoulder more; this action allows for the lubricating synovial fluid to being flowing again and work its way into the shoulder capsule. As the shoulder moves more, scar tissue begins to break up and becomes reabsorbed by the body.
Frozen Shoulder Diagnosis
After discussing the symptoms with you, your physician will test your range of motion to see where the limitations in movement occur and assess the pain you are feeling. Frozen shoulder doesn’t allow for a great range of motion, either passively – when someone else moves your shoulder – or actively – when you move your own shoulder.

X-rays or magnetic resonance images (MRIs) may be used to rule out other potential causes of your pain and restricted movement, such as arthritis or a torn rotator cuff.
What is the best treatment for a Frozen Shoulder?
Frozen shoulder doesn’t heal overnight, so patience is required; full recovery can take up to three years. Many patients respond to simple treatments to control pain and restore motion. The goal of treatment is to alleviate pain and restore motion with the help of physical therapy.
Initially, assistance comes in the form of pain management. Your physician will probably suggest a non-steroidal anti-inflammatory pill that is available over the counter: Aspirin, ibuprofen (Advil, Motrin) or naproxen (Aleve, Naprosyn). Gentle massage may also be useful.
If you don’t respond to the non-prescription painkillers, your doctor may inject a corticosteroid into the shoulder joint or the surrounding tissue.
Concurrently, you should be working with a physical therapist to stretch the joint capsule and, later, to strengthen the surrounding muscles. Physiotherapy is a major key to recovery; your physiotherapist will determine how far you can push yourself and teach you frozen shoulder exercises that you can ultimately practise at home, including both stretches and range of motion exercises for frozen shoulder. Sometimes, heat is applied to loosen the shoulder prior to exercise.
Surgery for Frozen Shoulder
In extreme cases, surgery may be required to loosen the shoulder capsule. This most commonly means either manipulation under anesthesia or arthroscopic surgery or a combination. During manipulation, the doctor forces shoulder movement, tearing scar tissue and allowing healing to begin. Arthroscopy requires small incisions to cut through the joint capsule to loosen it. Post-op rehab physical therapy is necessary after frozen shoulder surgery to maintain the gains that it achieved.
If you suspect that you are suffering from frozen shoulder, consult with your physician so that the proper course of treatment can be followed. After all, it’s no fun to ask for help in reaching objects on a high shelf or putting on your coat.
Suffering from a FROZEN SHOULDER INJURY?
Intimidated by the Gym?
Working out at a gym is a normal, and often even daily route for many Canadians. Some go to the gym to maintain a healthy exercise routine, others work on strengthening and toning their muscles, enhancing their endurance on a treadmill or exercise bike, or head do the gym as part of a weight-loss program. Many tend to the gym to perform their exercise routines that have been put together for them by their physiotherapist to treat certain conditions.
For those that go to a gym regularly, it seems very natural, and they are completely at ease with the gym environment and how to use the equipment. However, a recent Ipsos Reid Poll shows that many Canadians are actually intimidated by the gym, amongst those, many British Columbians. While some are afraid other people will watch them, others feel too overweight to go to the gym.
Find out more in our “Intimidated by the Gym?” Infographic:
Feeling intimidated about an EXERCISE PROGRAM?
15 Interesting Foot Facts
Look down at your feet, and, most likely, what you’ll see is 10 toes wriggling or flexing. Now, if you had X-ray vision like Superman, you’d soon realize that there’s much more to your feet than meets the naked eye.
According to the American Podiatric Medical Association, your feet are a marvel of engineering that, as a pair, contain more than 50 bones – about one quarter of all the bones in your entire body! Working together with those bones are 60 joints and more than 200 muscles, tendons and ligaments that allow your feet to move.
Given their complexity, it’s not surprising that your feet can give you trouble. After all, they have a tough job. Foot pain and a sore back are very common conditions!
An average day of walking around pounds your feet with hundreds of tons of force – and that’s not taking into account your exercise regimen, whether your job requires you to stand all day or whether you’ve squashed your feet into shoes that are a bit too small because they look stylish.
See our infographic for 15 surprising and interesting foot facts:
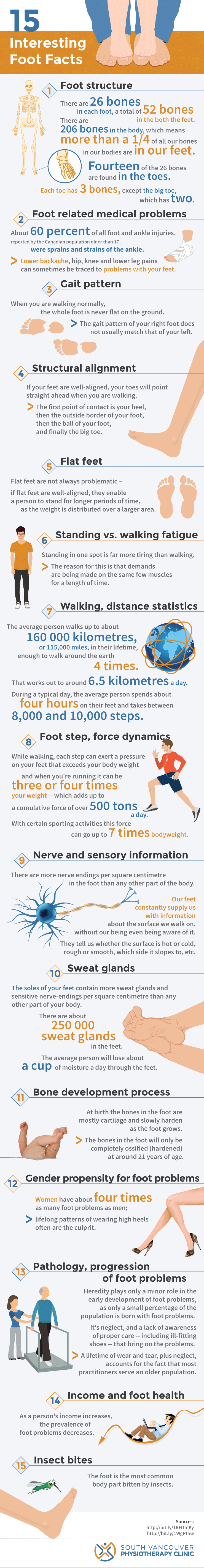
Embed This Image On Your Site (copy code below):
Suffering from FOOT PAIN or a SORE BACK?
How to Improve Posture - Seven Tips
Everyday activities such as sitting on office chairs, standing, sleeping or carrying a bag on the same shoulder can cause poor posture. Poor posture can create pain issues in your neck, back, and shoulders. Thankfully, there are steps you can take to improve your posture. By making a few adjustments, you can address poor posture and eliminate the pain caused by it.
How to make posture a good habit
[divider style=”empty” margin_top=”30px” margin_bottom=”0px”]
1. Keep your body aligned while sitting and standing
Sit up straight while in a chair, keep your hips, shoulders and ears aligned in one vertical line. Try to avoid crossing your legs, hunching shoulders or looking down at your screen. Sitting on a balance ball can help improve your posture by using your natural balance. When standing, distribute your body weight evenly between the front, back and sides of the feet. Being aware of how you are holding your body and taking the time to adjust throughout the day will help keep your posture in check.
2. Utilize posture friendly props and chairs
- Minimize back strain by using bags or backpacks that are designed to evenly distribute weight and reduce back strain.
- Avoid straining your neck with proper placement of your computer screen. Purchasing a monitor shelf that raises the screen to eye level will help reduce strain on your neck.
- Using lumbar back pillows when sitting or driving can create ergonomic support for your lower back and ease the strain on your overall body.
3. Take a break and move!
Slouching is a result of your muscles tiring and is where poor posture becomes more likely, resulting in extra pressure on the neck and back. Take a break every 30 minutes for two minutes and stretch, stand or walk.
4. Wear supportive footwear when standing
High-heeled shoes change the body’s centre of gravity and negatively affect back support and posture. Choose supportive shoes when you know you will be standing for extended periods of time. For those in jobs that require standing for an entire shift, supportive orthotics may be necessary.
5. Think good posture when lifting
When lifting, maintain good back posture to avoid injury. Good back posture includes looking forward, bending at the knee and keeping your back straight. Back injuries are commonly caused by twisting or lifting and occur during awkward movements.
6. Keep good posture while sleeping
If you are waking with a sore back or neck, there are many things to consider posture-wise while sleeping that could help:
- Choose a firm mattress for the best back support
- Sleeping on your side or back is better on your spine than stomach sleeping
- If you sleep on your side, placing a flat pillow in between your knees will keep your spine straight
- Use a pillow that provides proper alignment. You don’t want your head to be tilted upwards or downwards but in a neutral position.
7. Try and adopt an overall relaxed posture
There is such a thing as trying too hard. Keeping your body in a stiff, unnatural position to maintain good posture can create more pain as tense muscles put your body out of alignment. Keeping your body relaxed will lead to less stiffness over time.
There are many ways to help yourself when it comes to improving your posture. If you find you need assistance, your physiotherapist can design a customized treatment plan for you to get your body properly aligned again.
Suffering from INJURY due to poor posture?
Why Women Should Do Physiotherapy in Pregnancy
Visiting a physiotherapist while prenatal, pregnant or postpartum can help both with the prevention and treatment of pain and pelvic issues caused by pregnancy as well as aid in recovery after childbirth.
Physiotherapy in Pregnancy
Here are some of the reasons why women should visit a physiotherapist in pregnancy:
Physiotherapy for Pregnant Women
Physiotherapists can work with women to help them prepare their bodies for pregnancy including ensuring the body is aligned and ready to carry a baby. If your body is already compensating for previous injuries, pregnancy can add further strain and pain. Physiotherapy can also teach pregnant women how to correctly perform Kegel exercises which will help strengthen the pelvic floor in preparation for childbirth.
Kegel exercise consists of repeatedly contracting and relaxing the muscles of the pelvic floor.
Physiotherapy Assists with Posture Changes during Pregnancy
Pregnancy puts a huge strain on a woman’s body. The physiological changes that come with pregnancy include an increase in body mass, retention of fluid and laxity in supporting structures.
These changes cause postural adaptations such as an alteration in the loading and alignment of the spine and weight-bearing joints that often cause back pain and pelvic pain that is associated with pregnancy.
Core stability training with a physiotherapist is one way to help prevent and treat back pain during and following pregnancy.
You Learn How to Push Correctly During Labour
Using their knowledge of the pelvic floor, physiotherapists can help teach women how to push effectively during childbirth. Pushing correctly will reduce the chances of pelvic floor trauma and subsequent problems.
Physiotherapy Assists with Pelvic Floor Rehabilitation
Throughout pregnancy and labour, a women’s pelvic health can be compromised. Physiotherapists have specific training to assess the muscles, connective tissues and nerves in the pelvic floor.
Some conditions that can arise from trauma to a woman’s pelvic floor include incontinence, pain during intercourse, and pelvic organ relapse.
After a woman has had a baby, an assessment and a plan for rehabilitation will assist in the recovery of her pelvic floor.
Want help preparing your body for PREGNANCY?
What To Do Following a Car Crash
Being the victim of a car crash can be a jarring and frightening experience. Whether it is a minor fender bender or a major motor vehicle accident, it is a scary and inconvenient occurrence, often leaving you with a feeling of “what now?”
Why Motor Vehicle Accidents Happen
Car accidents can happen due to several combining factors:
- Speed: speed kills, period. There are posted limits on all roads in BC for a reason; sadly not everyone abides by these limits. Speeding is one of the leading causes of car crash fatalities in the province. You can practice safe driving by slowing down, passing with care and keeping a safe distance between other cars.
- High-risk driving, such as pulling into traffic without giving yourself enough time or space, tailgating, or failing to yield, are all high-risk driving behaviours
- Distracted driving: Texting, talking on your phone without a hands-free device is distracting and contributes to accidents.
- Impaired driving: This is not only dangerous but also illegal. Always plan a safe ride home if you’ve been drinking. You’ll be helping to keep our roads safer for everyone.
What To Do Following a Car Crash?
Although you may be feeling frightened after a car crash, it’s important to stay calm and follow the protocol listed below. Ensure that you or anyone else involved in the accident does not require immediate medical attention. If anyone does require immediate medical attention, dial 9-1-1 for assistance.
If immediate medical attention is not required, usually emergency responders (such as police, fire and paramedics) will not attend the scene.
When the vehicles have been pulled over to a safe spot, or emergency personnel have secured the scene, and it is safe to do so, you will need to exchange the following information with the other party involved in the accident:
- The license plate number and the year, make, and model of each vehicle involved
- Your personal information, including your name, address, and driver’s license number
- The names and address of the owners of the vehicles (if you’re not the owner)
- The name of your insurance company
- Your phone number, if necessary
If there were any witnesses to the accident, be sure to get their names and any necessary contact information, such as phone number, email or address. Further, if the police are on the scene, be sure to ask for the police file number for your reference.
If you have a camera (e.g. on your cell phone), and if it is safe to do so, you should take pictures of the accident scene and surrounding area. Include the intersection or area of the road, any skid marks on the pavement, damage to all vehicles involved, and any visible injuries to yourself that have appeared (bruises or lacerations).
Once the scene has been secured and you are finished with all involved parties (witnesses and drivers) and emergency responders, you should seek medical attention to have your injuries assessed and documented by a medical professional. If possible, you may want to get a friend or family member to take you to the hospital, your doctor or a walk-in clinic.
Finally, after you have received the appropriate medical attention, contact your insurance company. If you get your insurance through ICBC, call the Dial-a-Claim service at 604-520-8222 (Lower Mainland) or 1-800-910-4222 outside of the Lower Mainland.
During this phone call, you will report the accident by giving the pertinent details about the accident, as well as a description of how the accident occurred. You will be assigned an ICBC claim number and an appointment to meet with an ICBC estimator and adjuster. The estimator will assess the damage to your vehicle while the bodily injury adjuster will discuss your injury claim with you.
Have you been INJURED in a car accident?
How to Prevent Falls in Seniors
Falls in elderly Canadians are one of the main causes of moderate to severe injuries, including sprains, fractures, and head traumas. According to research, one in three elderly Canadians fall each year, and often the result is an injury that can permanently reduce their mobility and independence.
The fear of falling can be detrimental to the social, physical and cognitive health of a senior. Normal activities that come from leaving the home and venturing out to participate in social events help maintain a senior’s health, muscle strength, and balance, among other benefits.
How to Prevent Falls in Seniors
The truth is that falls in seniors are preventable. Modifying the home and reducing hazards outside the home in the community can greatly reduce falls. It is also important to identify and be mindful of other risk factors, such as side effects of medication or physical weakness.
A physiotherapist can help to improve the physical components related to fall prevention and rehabilitation. Physiotherapists can assist the elderly in maintaining their muscle strength, coordination and flexibility to recover from injuries and in preventing falls in seniors from occurring.
An added benefit is their ability to educate seniors on hazards that may contribute to falls, as well as work with them to build and strengthen muscle tone and coordination. By reviewing a senior’s medical history, assessing their current physical condition, and doing a series of tests that measure strength and flexibility, the physiotherapist can create a comprehensive program that will improve the senior’s physical function.
Tips for Preventing Falls in Seniors
- Wear a solid, well-made pair of shoes that provide support and cushioning that is necessary for movement and walking
- Avoid any shoes that may be unstable or slippery, such as those with an open-toe or with high-heels or slippers
- Make sure areas of movement, such as stairwells and hallways, are well lit
- Use a walking aid, such as a cane or walker – and view them as a source of aid and strength, not weakness or embarrassment
- Ensure that the tips on canes and walkers are not worn and in good working order
- Sit, rather than stand, while getting dressed
- Rise slowly from sitting to standing or lying down to sitting to reduce possible dizziness or instability.
- Install handrails, if necessary, in bathrooms or hallways.
- Wipe up floor spills immediately.
- Don’t take unnecessary risks by standing on furniture or putting yourself into an unsafe situations; wait for help or use a secure stepladder.
- Ensure feet are well planted on the ground when getting out of a vehicle.
- Put everyday items at eye level so you aren’t reaching up to grab things.
- Be mindful around small children or pets, which can easily get underfoot and cause a fall.
Need help PREVENTING FALLS?
Preventing Winter Sport Injuries
During the winter months, people from all over the world participate in the popular winter sports of skiing and snowboarding. They are both fun and exciting winter activities, but each can also put you at risk for injury. There are many things that you can do for preventing winter sport injuries this winter season and maximize your time on the slopes.
Common Risk Factors for Winter Sport Injuries
In both sports, there are some common risk factors that can contribute to winter sport injuries:
- Fatigue due to skiing/snowboarding without rest
- Skiing/snowboarding above your ability level
- Improper/faulty equipment
- Dehydration/fatigue
- Skiing/snowboarding in out-of-bounds areas
- Failure to adhere to posted warning signs
- Not maintaining proper code of conduct/safe practices
In skiers, the most common winter sport injuries include:
- Knee injuries, including MCL and ACL, strains or tears
- Knee sprains
- Shoulder injuries from falls
- Broken leg
- Thumb or wrist injuries, also from falls
- Head or neck injuries (less common)
In snowboarders, the most common winter sport injuries include:
- Wrist and hand injuries due to the nature of falling while strapped into a snowboard
- Collarbone and shoulder injuries
- Head and neck injuries
Preventing Winter Sport Injuries
Here are some safety precautions that can be taken to help prevent winter sport injuries this winter:
- Prepare your body by warming up beforehand. For example, do some stretching and take a brisk walk to warm up your muscles, or start out on an easy run.
- Ensure you have proper equipment that fits your body and skill. Make sure ski/snowboard boots fit properly, bindings are in good working order, and ski length is appropriate for your height and skill level.
- Wear safety gear, such as a helmet, and wrist guards if you’re snowboarding.
- Be sure to practice proper skiing and snowboarding techniques. If possible, take lessons to learn these techniques.
- Stay on marked trails: Going off trail can take you into unsafe territory with unpredictable obstacles, such as trees, rocks, and debris.
- Rest if you’re tired, as many injuries happen when fatigued.
- Stay hydrated.
- If you’re skiing with others, be sure to stay together.
It’s also important to understand the physiology involved in snowboarding and skiing. They are both sports that require a good deal of leg strength and core strength to be effective. There are some exercises that will help you to prepare for a season of skiing or snowboarding, and strengthen your muscles to help preventing winter sport injuries. For example:
Double Leg Squats: in this exercise, you place your feet a shoulder width apart and squat down, keeping your heels on the floor. Stick your bottom out and focus on using your gluteal muscles to lift and lower your weight. Your shins should be parallel to one another, and you should be replicating the squatting position that you remain in for most of the time you are on skis. Do this for 10-15 repetitions holding midway through the squat. This exercise will help build your gluteal and quadriceps muscles – essential for skiing.
Side-to-Side Skaters: Stand on one leg and take a wide step to the side with your other leg; next, stand on that leg and take another large step back to where you were. Keep your pelvis level and ensure that your knees don’t buckle inward. Continue this exercise for as long as you can, or up to 3 minutes. The more slowly you go, the more difficult it will become.
Want help PREVENTING WINTER INJURIES?
Dealing with Strains
A strain is a stretched or torn muscle or tendon. Tendons are tissues that connect muscle to bone. A strain occurs when a muscle is stretched beyond its limits during the course of everyday activities like with a sudden lift or a twist during sport or while performing a work task. Strains can happen suddenly or develop over time like in the case of repetitive strain. Back and hamstring muscle strains are common. Typically the local area is painful, swollen, red and bruised and the muscle may spasm and become weak.
Your physiotherapist can work with you to minimize the amount of damage from an injury and speed the healing process. Small and simple changes to your movements, combined with adequate muscle strength and following the Physio-4 for Strains, can prevent muscle strains in the long run and keep you moving for life.
4 Tips to Minimize Damage and Speed the Healing Process from Strains
1. Early on, relative rest is key. In the early stages of treating a strained muscle, you should be resting the muscle to ensure the small muscle fibers that have been damaged have time to heal properly. Do not stretch in the early stages. You can use heat or ice for pain management. Avoid any painful activities such as the one that originally caused the injury. After a comprehensive assessment your physiotherapist will guide you by appropriately increasing your activities in order to avoid re-injury. Your physiotherapist may also use treatments such as electrotherapy, acupuncture and manual therapy to reduce healing time.
2. Protection is sometimes necessary. The challenge of having an injury is that we still need to use the injured area with everyday life. This sometimes doesn’t allow our injury to heal so that’s when we use splinting or braces. Hand strains, for instance, can take a long time to heal since it is hard to rest this area of the body. Your physiotherapist will tape or brace just the strained area so that you can keep moving while your body heals. They will also advise when this can be discontinued to allow you to progress beyond the acute stage.
3. Move Early to Restore Normal Function. Strained structures need to be strengthened while balance and dexterity are improved, so early and limited movement is extremely important. As you heal, practice skills as simple as holding chopsticks or changing direction quickly on a soccer field. Small and simple changes to your movements, combined with adequate muscle strength, can prevent muscle strains in the long run. Your physiotherapist will educate you on how to prevent re-injury and guide you along the path back to your active lifestyle.
4. Not all strains are equal. The local area of a muscle strain is painful, swollen, red and bruised and the muscle may be weak and painful to use. Treatments for strains are individualized, based on the mechanism of injury, the degree of strain, the specific muscle at fault and the functional goals of the individual. Your physiotherapist will help you differentiate between a mild muscle strain that can be treated conservatively, versus a severe strain such as a complete tear that may require further medical attention. And your physiotherapist will correct any biomechanical issues and create an individualized exercise plan, including stretching and strengthening at the appropriate time intervals.
Physiotherapists are the rehabilitation specialists recommended most by physicians. They are university-educated health professionals who work with patients of all ages to diagnose and treat virtually any mobility issue. Physiotherapists provide care for orthopedic issues such as sport and workplace injuries, as well as cardiorespiratory and neurological conditions. As Canada’s most physically active health professionals, BC’s physiotherapists know how to keep British Columbians moving for life.