What is a Groin Injury?
The groin, perhaps because of proximity, isn’t a region that is mentioned often in polite conversation. In fact, although it is likely we can all refer to its general location, we have probably never tried to pinpoint it or define it.
However, it’s a challenge we’ll take up here, because the groin is an area of the body that is prone to injury – groin strains are common, but before we can treat them, we must be clear about what we’re discussing.
Where is your Groin?
Let’s take a look at groin anatomy. The groin, also called the inguinal region, is the area of the body between the abdomen and the thigh on each side of the pubic bone. It contains the adductor muscles of the hip.
Usually, groin strains, which are muscle tears, take place in the upper groin area near the pubic bone or at the front of the leg. Depending on their seriousness, groin strains are classified by grade.
A Grade 1 strain is a minor tear to the muscle that causes some pain or tenderness; a Grade 2 strain is the tearing of a larger percentage of your muscle fibres that causes tenderness, pain, weakness and, possibly, some bruising; while a Grade 3 strain is a severe tear that results in a lot of pain and bruising.
Causes of Groin Pain
A groin injury can occur when there is any forceful leg movement: changing directions while running, jumping or kicking, for example. A direct blow to the area, a fall or any movement that moves the groin at an unusual angle may cause a strain.
Athletes are always at risk for groin strains, which can occur while skating, kicking a ball or playing basketball. A groin strain may also result when you are pushing, pulling or lifting heavy objects. It may also result from overuse of your muscles or from exercising without warming up.

Groin Strain Symptoms
When you strain your groin, you will generally feel a sudden pain accompanied by a snapping sound when you move your leg or your hip. Swelling and bruising will probably follow quickly. You may also have spasms and feel sharp pain if you try to lift your leg or bring your legs together.
With a Grade 1 sprain, you’ll be able to walk normally and the use of your leg won’t be impaired. A Grade 2 sprain will commonly lead to a limp and restricted use of your leg. With a Grade 3 strain, it will be very painful to put any weight on your leg and you will have difficulty using it. There may even be a dent in the muscle that is visible under the skin at the tear site.
How to treat a Groin Injury
Once you experience groin pain and realize you have sustained a groin injury, you’ll want to begin the standard RICE treatment — rest, ice, compression and elevation – and continue it for the first 24 to 48 hours. Try not to put weight on your leg and apply ice to the area for 15 to 20 minutes every two hours. Apply an elastic bandage to the area for compression and ensure it is cushioned by pillows to elevate it.
To get relief from the pain in your groin area, you can take an over-the-counter non-steroidal anti-inflammatory medication, such as acetaminophen or ibuprofen.
Your physician, after diagnosing the injury, should refer you to a physiotherapist for treatment. In assessing your injury, the physiotherapist will ask you questions about how the groin injury occurred and what you felt at the time.
They will test your muscle strength, move your leg away from your body and gently touch you to determine exactly where the tear has occurred. He or she may also do additional testing to ensure that your hip or your back aren’t injured, too.
Following the assessment, your physiotherapist will design a program of rehabilitation and recovery for you to allow you to heal quickly and return to normal activity as soon as possible. Your program will include exercises and stretches for groin pain that will improve strength, improve motion and hasten your recovery.
Prevention of Groin Injuries
You can certainly take steps to prevent a groin injury, although there are no guarantees, especially if you are involved in sports. Warm up your muscles by stretching or doing light exercise before participating in a game or more intense exercise.
If you don’t exercise regularly, take things slowly. You don’t want to exceed your comfort level or injury can result. Try to keep your level of exercise consistent, rather than doing some intense exercise on Monday and not exercising at all for three or four days. Take a hint from professional athletes who generally train year-round.
If you keep your leg muscles strong, you’re less likely to experience a groin injury.
Let's get you some relief for your Groin Injury!
What is a Heel Spur?
Do you suffer from heel pain? If so, you’re not alone. Unfortunately, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it. When you continue to use a sore heel, it will only get worse and could become a chronic condition leading to more problems.
It shouldn’t hurt to get to your feet in the morning or walk throughout the day. If you notice a sharp, stabbing sensation in your heel with each step you take, you may be suffering from heel spurs.
How do you know if you have a heel spur?
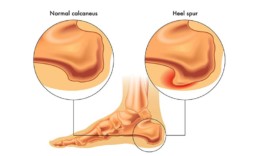
Heel spurs develop over time; they don’t magically appear. Repetitive strain on your muscles and ligaments in the foot and heel can lead to a heel spur, a bony buildup of calcium on the heel that can form and cause pain.
There are two types of heel spurs: an inferior calcaneal spur, which results from ongoing stress to the bottom of the heel and grows between the heel and the arch of the foot; and a posterior calcaneal spur, which is the result of repeated trauma to the back of the heel where the Achilles tendon is attached.
The posterior calcaneal type of heel spur is often visible to the eye and can be easily felt, but the inferior calcaneal spur is trickier to diagnose, because the pain it causes can be mistaken for plantar fasciitis.
Generally, an X-ray is required to ascertain that a heel spur is, indeed, the cause of the pain you are experiencing.
What causes heel spurs?
Common causes for heel spurs include heel bruising, arthritis, shoes that fit poorly, the effects of excess weight, footwear with minimal support (e.g., flipflops) and gait issues that put too much pressure on the heel bone and surrounding ligaments and nerves.
Aging can also be a contributing factor, because the plantar fascia become less flexible and the heel padding becomes thinner. Flat feet or high arches may also lead to heel spurs, as can diabetes or work that requires you to spend most of the day on your feet.
Heel Spur vs Plantar Fasciitis
Heel spurs often co-exist with cases of plantar fasciitis. The plantar fascia are the fibrous tissues that run from the heel to the ball of the foot and inflammation of these tissues is called plantar fasciitis. However, plantar fasciitis can be cured, but once heel spurs develop, they remain in place, although their impact can be minimized.
Heel spur sufferers may experience a sharp, knifelike pain when they stand up; the pain generally lessens and becomes a dull ache. You may feel heat radiating from the area and see inflammation and swelling.
Walking barefoot may be difficult due to tenderness at the bottom of the heel. Often, the heel spur itself is not the cause of the pain; the pain comes from the injury underlying it.
Can a heel spur go away on its own?
As mentioned, heel spurs may be easily confused with plantar fasciitis, so your physician will generally request an X-ray before making a diagnosis. Heel spurs don’t dissolve or disappear, but you can mitigate the pain and discomfort they generate.
How to relieve heel spur pain
Your physician may suggest one or more possibilities to relieve heal spur pain. The easiest is the use of over-the-counter pain medications, such as ibuprofen, acetaminophen or naproxen. Icing your heel will also help reduce any swelling or inflammation.
Heel spur exercises
Physiotherapy is another useful option. Your physiotherapist will do an analysis of your gait and can prescribe a course of exercises that will help correct any imbalances that allow your heel spurs to grow. They may also use a combination of manual therapy and ultrasound to break down calcification. Acupuncture may also be employed to help reduce pain. To reduce the stress on your foot’s muscles and tendons, your physiotherapist may use strapping or taping techniques in the area.
Orthotics for heel spurs
Your physician or physiotherapist may also prescribe custom orthotics, inserts that are placed in your shoes to assist in correcting your gait and suggest that you wear cushioned sports shoes to alleviate pain.Custom orthotics often have a well cut in them to provide extra cushioning to the affected area to reduce the impact of walking or being active on your heel.
How long does a heel spur last?
Most sufferers of heel spurs recover from the pain and discomfort with nonsurgical treatments. However, if the discomfort persists after nine to 12 months, surgery may be necessary.
Remember: a heel spur is a chronic condition, so it will be up to you to manage it. By following your physician’s recommendations and doing the exercises prescribed by your physiotherapist, you should eventually be able to forget that they exist.
Let's get you some relief for your Heel Spur!
Why is Core Stability important?
Your core refers to the midsection of your body, front, rear and sides; it connects the upper and lower regions of your body. The core’s major muscle groups include the transversus abdominis (your six-pack abdominal muscles), the pelvic floor muscles, the internal and external obliques, the rectus abdominis, the multifidus, the erector spinae, and the diaphragm, which is crucial for breathing.
The core supports your spine and pelvis and is integral to motion, transferring force from one area to the other. Having a strong core is important for movement, because weak or inflexible core muscles can interfere with the proper functioning of your legs and arms. Strong core muscles also provide you with balance and stability and help prevent falls and injuries.
What Is Core Stability and Why Does it Matter?
Core stability refers to the ability to keep your spine from moving during physical activity, such as walking, running, swimming, etc. Your core helps you control your body effectively, helping you use your arms and legs to the best advantage and preventing your spine from bending or flexing unintentionally. Core stability is important because stability is crucial to your everyday activities.
Signs of a Weak Core
If you haven’t really thought about the importance of core strength until now, it’s time to pause and assess yourself. If you have a weak core, you needn’t simply sigh and fret; you can do core stability exercises to strengthen it.
There are a number of signs of a weak core. One of the major indicators is lower back pain that isn’t the result of another back issue. You need strong muscles surrounding your spine in order to properly support its vertebrae and discs. Without them, the forward curve of a normal spine won’t be possible and you may have pain in the surrounding tendons and muscles.
Another indicator is poor posture. Your spine and pelvis are held in place by the muscles in your abdomen and lower back. If they aren’t strong, your posture will suffer and the resulting slouch will strain muscles. Sitting or standing erect for long periods of time will be problematic. Often, people with lower back issues also have posture problems and vice-versa.
Strong core muscles are the key to stability, so if you are having trouble with your balance, your core may be the weak link. Test yourself by standing on one leg with your eyes closed for ten seconds; try this with each leg. If you can’t hold the position, it’s a sign that your core needs strengthening. If you stumble, a strong core can help you remain upright, so it’s important to exercise those muscles.
The hollowing test is another way of checking your core strength. Take a deep breath and pull your stomach muscles back toward your spine as you exhale. If you can’t manage to hold them there for 10 seconds, it’s another indicator that more core strength is required.
If you have ever practised yoga, you are familiar with the plank position, one that challenges your abdominals and tests your core strength. Try it by assuming doing a push-up, resting your weight on your arms, elbows and toes with your hips held level and steady. If you can’t remain in this position for 50 seconds, guess what? Your core needs strengthening.
Finally, general muscle weakness may be an indicator of inadequate core strength. Your core provides the power for motion and stability, too. If your arms and legs aren’t being accommodating, it may be due to a weak core.

Why is Core Stability Essential for Seniors?
Core stability is integral to a wide range of daily activities, from walking to reaching for cans in the kitchen cupboard. It underpins almost everything you do throughout the day, so it is crucial to your quality of life.
A stable core allows you to have more control over your body, whether you are in motion or sitting still. A healthy core is important in preventing accidents and injuries; seniors are often vulnerable to falls, so stability is especially important as you age. A healthy core also helps you fight pain and maintain balance, co-ordination and good posture. It even assists with breathing and digestion.
If you’re determined to stay as healthy as possible as you age, having a strong, stable core is an essential ingredient.
Need to Strengthen your Core?
Rest, Ice, Compression, and Elevation - The RICE Method Explained
RICE is the acronym that stands for Rest, Ice, Compression and Elevation. It’s a mnemonic, or memory device, that helps you remember quickly what to do when injury strikes a ligament, a tendon or a muscle.
The RICE method can generally be used even before checking in with your physician or physiotherapist. It is generally effective if employed as soon as possible within the first 24 hours following injury and continued for up to 48 hours. It’s simple to do and the benefits are evident, because sprains are often painful and swell rapidly.
Rest
If you think you’ve sprained an ankle or pulled a muscle in your back, it’s time to stop any activity that aggravates the injury and causes you pain. Especially if it’s a limb, avoid moving it and keep weight off it to prevent further damage. Crutches or a brace may be necessary if your leg is involved.
You may be able to exercise other muscles to prevent de-conditioning, but handle the injured area with care; in fact, it would be wise to check with your physiotherapist to determine which exercises won’t be harmful under the circumstances.
Ice
Cold is useful for its ability to prevent or limit swelling. It can also numb the affected area, which is a blessing if you are in pain. In applying cold to the injured area, be sure the frozen item has no direct contact with your skin; place ice or a cold gel pack or frozen peas or corn – which mould nicely to the shape of an ankle or knee – in a dishtowel to protect your skin from freezer burn.
Try to apply the cold/ice to the injured area as soon after the injury as possible and continue to do so for 20 minutes at a time, eight times each day, for the first 48 hours.
Compression
Compression also helps decrease swelling in the injured area. Use an elastic or tensor bandage to wrap the affected area, but don’t make it so tight that you prevent proper circulation in the area. If you wrap it too tightly, you’ll probably see swelling BELOW the bandage. Other signs that the compression bandage is too tight include numbness, tingling, coolness or increased pain.
Use compression to treat your injury for 48 to 72 hours. If you have a more severe injury, your physician may suggest an air cast or splints to provide more support while assisting with compression.
Elevation
Elevation reduces blood flow to the injured area, consequently reducing swelling and keeping bruising down. Raise the injured area above your heart, if possible – especially when icing it – and cushion it with a pillow. Try to elevate the injured area for two to three hours daily.
Of course, depending on the injury, the RICE method is likely to be only the first stage in treating it. In general, you’ll want to have your physician assess the injury, especially if you can’t put any weight on the area or if the area is numb or misshapen. You may also want to take non-prescription non-steroidal anti-inflammatory drugs (NSAIDs) to relieve pain.
Once the swelling has gone down, your physician will probably suggest you see a physiotherapist to rehabilitate the injury through targeted stretching and strengthening exercises.
Let's get you back on track!
What is a Contusion?
There shouldn’t be any confusion about a contusion. In plain English, it’s a bruise. We’ve all had them, especially as children: bumping into the dresser in the bedroom or getting tackled on the soccer pitch, for example. Contusions are very common workplace injuries and sports injuries, almost as common as muscle strains. They can be painful, but generally, they’re not dangerous to our long-term health.
Contusion Definition
A contusion is an acute direct muscle injury result from blunt trauma to the tissue, accompanied by an accumulation of blood. You may sustain a blow in a sport or you may bump into a fixed object; either way, both your muscle fibres and small blood vessels (capillaries) become injured. Blood from the capillaries leaks out and settles under the skin, although the skin isn’t broken.
The size of the bruise depends on the force involved in the injury, as well as the cause. The greater the force or the larger the object involved, the bigger the contusion.
A contusion also may not be visible immediately; it may take time to develop. It also may not appear directly at the site of the injury, since gravity can send the leaking blood to the lowest portion of your limb; hence, trauma to the knee may result in a contusion near the ankle.
Contusion Symptoms
Bruises add a bit of colour to our complexions, albeit not the most attractive sort. The contusion will also change colour over time. Initially, a bruise usually looks red in colour due to the new blood leaking into your tissues. It contains both oxygen and hemoglobin, a protein that is rich in iron.
Shortly afterward, the blood loses its oxygen and your contusion turns a blue or purple colour. As the red blood cells break down, they leak hemoglobin and iron, often turning the contusion a darker purple or a black colour.
Since a contusion doesn’t usually involve muscle tears, you may be able to ignore it and continue on with work or a sporting activity. However, the area may be tender and there may be some swelling and soreness to the touch. Contusions do have an impact upon muscle function, so your range of motion in the area may be limited.
Contusion Treatment
When it comes to how to treat a contusion you’ll want to adopt the PRICE protocol in the first 72 hours following an injury that causes a contusion. PRICE is an acronym standing for protect, rest, ice, compress and elevate and is useful in controlling bleeding, pain and swelling. If the injury occurs during a sporting contest, stop playing immediately to prevent further damage.
The term, rest, is a relative one. You shouldn’t keep the area immobilized – it’s important to get it moving – but you should do so gently without exerting undue force.
Icing should be done on and off for 15 to 20 minutes at a time. The cold reduces pain while preventing additional tissue damage. Be sure to wrap your ice or cold pack in a towel to prevent damage to the skin.
Using a compression bandage can also assist in keeping swelling down and improving circulation, although it is important not to bind the contusion too tightly.
Elevation is also useful for 10 to 20 minutes at a time; it helps to reduce swelling and promote circulation and healing.
Once you get past the 72-hour mark, you’ll want to begin promoting movement and improving the function of your injured muscle. A physiotherapist can be very helpful at this stage in prescribing exercises that increase strength and pain-free range of motion.
These movements will help increase circulation and healing, clear the area of cellular debris and prevent the buildup of scar tissue. A physiotherapist may also employ hands-on techniques to speed recovery, such as massage, or electric modalities, such as ultrasound.
How Long does a Contusion Last?
You can expect a contusion to heal in about two to three weeks, depending on the severity of the injury. As you begin to heal, your physiotherapist will eventually introduce resistance exercises and sport-specific exercises that ready you for a return to sport, if that is your goal.

Complications
Most contusions are straightforward and heal as expected over time. However, in rare cases, there may be complications, especially with more severe contusions. You’ll want to consult with a physician if these develop.
Your contusion may develop a hematoma, or a blood clot, which feels like a hard lump in your muscle that is evident fairly early on in the recovery process. Generally, it is absorbed back into the tissue.
Once in a while, a contusion leads to deep vein thrombosis, a blood clot that forms deep in the veins. It is a very serious condition, because there is always a risk of a piece of the clot breaking off and travelling to the lungs.
You can help prevent such clots from forming by ensuring that you begin moving the affected area of the body early, regularly and gently.
Luckily, complications are, as noted, rare, and you should be healed and raring to go in a matter of weeks.
Do you need help with treating a contusion?
What is Whiplash?
In Canada, whiplash accounts for more than $2 million in insurance claims each year that cost the economy about $600 million in lost work productivity, sick leave and medical care.
Let’s take a look at some of the most common questions surrounding whiplash including:
- What is whiplash?
- What does getting whiplash mean?
- How do you know if you have whiplash? What does whiplash feel like?
- How long does whiplash last?
- What is the best treatment for whiplash?
What is whiplash?
The Physiotherapy Association of British Columbia defines whiplash as “an acceleration-deceleration mechanism of energy transfer to the neck. It may result from rear end or side impact motor vehicle collision but can also occur during diving or other mishaps. The impact may result in bony or soft tissue injuries (whiplash injury), which in turn may lead to a variety of clinical manifestations called whiplash-associated disorders (WAD).”
What does getting whiplash mean?
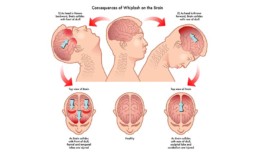
Anatomically speaking, the mechanical forces that occur when the head and neck are whipped forward and back place major stress on the cervical spine. As the head is thrown backward, then forward, the cervical spine is first hyperextended and then hyperflexed; these movements are outside the normal range. The discs can rupture and soft tissue damage can occur. The muscles and ligaments in the neck can become stretched, nerves may be damaged and, in rare cases, bones may break.
Although motor vehicle accidents are the most common cause of whiplash, it can result from a number of other activities that can yield a strong impact on the cervical spine, such as contact sports like hockey, football, rugby and boxing; roller-coaster rides; horseback riding or bicycling accidents. Any direct hit to the head by a large, heavy object may lead to whiplash.
How do you know if you have whiplash?
Whiplash injury symptoms may not appear immediately upon impact. They usually develop within 24 hours of injury, but they may disappear and return after a day or two. They are usually confined to the upper, or cervical, spine and to the middle of the back (thoracic spine), but pain may radiate into the arms, shoulders and head.
If you have whiplash, you may have restricted movement in your neck and your head may feel heavy. Common symptoms include neck stiffness and decreased range of motion; an aching or painful neck or back; fatigue; arm pain and weakness; headaches that generally attack the base of the skull; shoulder pain and stiffness; and jaw pain. The pain is usually dull but may worsen depending on your movements.
Whiplash sufferers may also experience cognitive symptoms as a result of their injuries. You may suffer from ringing in your ears; memory problems; dizziness; difficulty sleeping; irritability; difficulty concentrating; and blurred vision or other visual disturbances.
If your symptoms are painful, spreads to the shoulders or arms, causes numbness or tingling or interferes with everyday activities, you should seek treatments. Medical advice and physiotherapy can help you get back on track.
How long does whiplash last?
When you meet with your physician and with your physiotherapist, it is useful for them to have a catalogue of your symptoms and the movements that create pain.
Generally, it takes about three months for the neck to heal completely, although the pain will subside much sooner.
What is the best treatment for whiplash?
After the initial injury, you may want to ice your neck and consider non-steroidal anti-inflammatory medicine that is available over the counter.
In the past, it was believed that rest was essential to recovery from whiplash and sufferers were given foam neck collars to wear in order to prevent movement. However, it has been demonstrated that this approach does more harm than good; the neck needs to be strengthened in order to aid recovery.
Your physiotherapist will help you strengthen your neck muscles and make them more limber by giving you exercises targeted to your whiplash injury. Not only will this help you heal, but it will make you more resistant to future neck strain.
Starting physiotherapy and its attendant neck exercises as soon after injury as possible will help you recover completely. It will also forestall you from adopting poor posture and overarching your neck to avoid pain. Doing so can create long-term neck problems.
In addition to prescribing a course of whiplash exercises, your physiotherapist may use ultrasound therapy to improve function and decrease pain, while enhancing cartilage repair. Deep tissue massage may be used to treat muscle stiffness that results from the tension that can result from whiplash, and electrical stimulation can assist in relaxing muscles that are tight or having spasms.
As you heal from whiplash, you’ll undoubtedly be eager to prevent it from occurring in the future. If your injury is related to an automobile accident, be sure to buckle your seatbelt when driving and to adjust your headrest to the proper height to give yourself the best chance of avoiding whiplash during an impact.
Are you suffering from whiplash?
Abnormal Gait and Balance Problems
Most of us give little thought to walking; it’s movement that seems to come as naturally to us as breathing – except when it doesn’t.
Walking takes strength, balance, sensation and co-ordination. Think about babies: first, they gain enough strength to raise themselves to their hands and knees to crawl. Next, comes pulling themselves up by grabbing a chair. Finally, they merge their newfound strength with co-ordination and manage to propel themselves forward, albeit awkwardly. It takes time and practice for them to find a natural gait.
As adults, we tend to forget how intricate this process is and how easily it can be disrupted. However, normal gait and balance rely on the proper functioning of various body parts, including the ears, eyes, brain, sensory nerves and muscles.
Injuries or problems with any of these parts can result in an inability to balance or to an unsteady gait, which can lead to falls or injuries if the causes and symptoms aren’t addressed.
Common Causes for Abnormal Gait
If an injury or illness has impaired your ability to walk normally, you may need gait training to improve your motion. Potential causes of problems with gait and balance include:
- Aging: With a natural decrease in strength and flexibility comes impairment to your balance.
- Musculoskeletal Problems: If your range of motion, strength, endurance and mobility are impeded for any reason, your gait may be affected, since you need a certain level of balance and strength to walk properly.
- Impaired Cognition: You are less able to adapt to a situation if your judgment or safety awareness decreases, your attention is poor or you process information more slowly than before.
- Impaired Neuromuscular Responses: Disruption in the signals between the brain and the muscles can affect gait and balance. The disruption can result from a variety of issues, such as a stroke, Parkinson’s disease or multiple sclerosis.
- Impaired Sensory Processes: If your body’s sensors are unable to collect information about the environment, it can lead to balance and gait issues. Sensory disabilities may be caused by glaucoma, cataracts or diabetic retinopathy, to name just a few possibilities.
Gait Analysis
Your physiotherapist may diagnose your gait as abnormal after reviewing your medical history, discussing your symptoms and doing a walking gait analysis. She or he may use a gait scan device to assess the biomechanical function of your feet.

Gait and Balance Training
Gait and balance training is a type of physiotherapy that helps you learn to walk normally again. The benefits of gait and balance training include:
- Improving your balance and posture;
- Strengthening your joints and muscles;
- Developing muscle memory;
- Increasing your endurance;
- Retraining your legs to participate in repetitive motion; and
- Increasing your mobility while decreasing the risk of falling.
It also offers other health benefits; because you are mobile rather than stationery, it can improve your overall health, prevent increased osteoporosis and keep heart disease at bay.
Your gait and your balance are inextricably linked, both relying upon the body’s cognitive functions, the eyes, the ears and joints, muscles and nerves. Gait and balance training helps these parts work in harmony.
Gait and balance training is also very helpful to people recovering from a variety of health issues, such as a spinal cord injury, a joint replacement or a stroke. Learning to walk properly again requires determination and practice. Training also helps prevent injury, assists with posture and keeps related aches and pains to a minimum.
Before you start gait and balance training, you must be healthy enough to take part in physical activity and your joints must be strong enough to support you. The activities your physiotherapist will instruct you to do will depend on your diagnosis and physical abilities. Gait training exercises often include walking on a treadmill, combined with strength and mobility exercises.
Orthotics
In addition to your gait and balance training, your physiotherapist may suggest custom orthotics for your shoes. Custom orthotics are not the casual shoe inserts that you can buy at any drugstore to add extra cushioning to your shoes. They are custom-made, prescription medical devices that you wear inside your shoes to correct biomechanical foot issues – unstable or impaired gait when walking or running. These prescription inserts are useful in helping improve your gait and correcting the appropriate problem.
If you’re having trouble walking or are recovering from an injury, it is worthwhile to consider gait and balance training to get you back on your feet and on the right track.
Let's get you back on your feet!
What is Degenerative Disc Disease
The discs that reside in our spinal columns are a vital part of our anatomy, acting as shock absorbers for our vertebrae and allowing our spines to bend and twist. These discs are located between vertebrae and are actually tire-shaped pieces of rubbery cartilage with gelatin filling the hole.
Degenerative Disc Disease Causes
The prevalence of disc degeneration in people under the age of 50 has been shown to be 71 per cent in men and 77 per cent in women; for those over 50, it is present in 90 per cent of both men and women.
So lets take a look at some of the degenerative disc disease causes. As we age, our discs naturally degenerate. They lose fluid, making them flatter and narrowing the distance between our vertebrae. This means that the discs are less able to absorb shocks and render us less flexible.
The outer layer of the disc may also be subject to tiny tears or cracks, allowing the gelatin in the centre to seep out. This may cause the disc to bulge, rupture or break into pieces. Bone spurs may also form or the disc’s rough surfaces may rub against each other, given the decreased space between them; this may result in pain and inflammation.
In addition, the nerve roots, the points where spinal nerves leave the spinal column to extend to other body parts, may get irritated or become compressed. The condition and these related maladies are lumped together under the term degenerative disc disease (DDD).
Disc degeneration doesn’t always lead to tearing and subsequent pain. It is most likely to do so if you have a history of smoking; do heavy physical work; don’t get much exercise; or are obese.
Symptoms
There are various ways the discomfort of degenerative disc disease pain can manifest itself.
- Cervical Degenerative Disc Disease Symptoms. You may have back or neck pain that travels to the extremities; it can be mild or severe. You may find that your arms and shoulders are numb or tingling if the degeneration affects your cervical spine.
- Lumbar Degenerative Disc Disease Symptoms. If your lumbar spine is affected, you may have numbness in your legs, back or buttocks. If your ribcage hurts, your thoracic spine is likely responding to DDD. Bending over, reaching up or twisting may increase your pain, and it may worsen if you remain in one position for a long period of time. It may also be worse early in the morning.
The onset of pain may result from a major injury, such as a car accident, or a minor injury, such as falling from a stepping stool. However, it may also appear for no apparent reason.

How to Treat Degenerative Disc Disease
If your physician suspects that you have degenerative disc disease based on your symptoms, he or she may try to pinpoint the source of your pain; measure the range of motion of your spine, your arms and your legs; perform muscle strength and sensation tests to determine if a nerve is affected; and examine your posture and observe your gait.
So what is the best treatment for degenerative disc disease?
At home and at work you can get some pain relief for degenerative disc disease by applying heat or cold to the affected areas and take acetaminophen or a non-steroidal anti-inflammatory medication.
To achieve ongoing relief, physical therapy is the most common treatment. It helps in managing degenerative disc disease pain and improving range of motion, strength and flexibility. It assists patients in strengthening muscles that can help assume some of the load previously handled by the discs; it also increases blood supply to the injured area, bringing more oxygen and nutrients that can assist in repairing the damage done.
Degenerative disc disease exercises may include stretching and flexibility exercises that help you to improve movement in your joints and muscles, which generally aids in pain relief.
Strengthening exercises will strengthen both your core, which provides support to your spinal joints, and your extremities, which can assume some of the workload usually done by the spinal joint. Aerobic exercises may also be added to the program, since they improve mobility, relieve pain and help you maintain a healthy weight.
In addition, your physiotherapist may use spinal traction and some hands-on techniques, such as massage, to loosen tight muscles and stiff joints so they can move better. He or she will also give you instructions about sitting, standing, bending and sleeping properly to ease your pain.
If none of these methods produce results, talk with your doctor. In severe cases, surgery may be required.
Remember: disc degeneration is a normal part of aging; you can’t prevent the march of time but you can manage the changes with proper advice from trained professionals.
Let's get you some relief!
How to Get Rid of Muscle Cramps
Our muscles are the body’s gateway to movement. They are the only tissues in our body that can contract and move the other parts of our body, so we rely on them heavily.
It is skeletal muscles that allow for physical motion. These striated muscles are attached to bone in at least one place, and many reach across a joint and connect to bones at each end. They are the key to all of our conscious movements.
Muscle Cramps
Given our reliance on muscles for movement, when a muscle cramps, we’re dismayed, because, for a brief period, they don’t function. A cramp is a tightening or painful, strong contraction of a muscle that happens suddenly and involuntarily and lasts for a few seconds to a few minutes. It prevents the muscle from functioning properly.
Most people experience muscle cramps in legs, calfs, and feet. They may manifest themselves as a lump of hard tissue visible under the skin’s surface. Some people are prone to muscle cramps at night – the tightening of muscles in the calf, thigh or foot that often occur as they are awakening or falling asleep.
What Causes Muscle Cramps?
While all of the causes of muscle cramps aren’t known, they are sometimes related to an underlying medical condition, such as nerve compression, mineral depletion and inadequate blood supply. Generally, people are more susceptible to muscle cramps as we age, because they lose muscle mass and the remaining fibres are overstressed more easily.
- Muscle cramps can happen if a muscle is injured or overused or they can occur during exercise.
- Mineral depletion, often due to the use of diuretics prescribed for high blood pressure medication, can lead to cramps, as can a dearth of calcium, potassium and magnesium in your diet.
- Muscle cramps in pregnancy are common due to the need for additional minerals in the diet during pregnancy.
- If you are dehydrated or exposed to cold temperatures, especially cold water, your muscles may contract.
- Standing on a hard surface or sitting in one place for an extended period of time can cause cramps, as can sleeping with your legs in an awkward position.
- In addition, if you are taking certain medications, such as birth control pills, or steroids, you may be more prone to muscle cramps.

Home Remedies for Muscle Cramps
For most people, you can address the cramps yourself using a variety home remedies for muscle cramps:
-
- If you find one of your muscles cramping, first try massaging it and stretching it.
- Heat may alleviate some of the discomfort, so take a warm bath or shower or apply a heating pad to the affected area.
- If you’d prefer to try ice, use an ice pack on your muscle, but don’t place it directly on the skin; use a dishtowel as a barrier.
- Taking non-steroidal anti-inflammatory medication may also help ease the pain, and these are readily available over the counter.
- Finally, ensure that you aren’t dehydrated; drink fluids. Sports drinks can be helpful in easing leg cramps.
- If your cramp is a leg cramp, try jiggling your leg or walking around. You should also stretch your calf muscles, either while standing or sitting.
Generally, your cramps will ease as a result of one or more of these home remedies. However, consider seeing your physician if the cramps don’t improve with self-care; occur frequently; prompt redness, swelling or changes to your skin; cause severe pain; or don’t seem to bear any relation to exercise, overuse or any particular cause.
How to Prevent Muscle Cramps
If you want to prevent muscle cramps, staying hydrated is your first line of defence. Drinking fluids allows your muscles to contract and relax. Maintain a healthy diet, rich in magnesium, potassium and calcium.
Stretching both before and after exercising is also a good preventive measure. You may want to consult a physiotherapist about the best prevention exercises to use.
Let's get rid of those muscle cramps!
How to Treat a Calf Strain
The area of the leg behind the knee that reaches to the ankle is called the calf, deriving from the Old Norse word, kalfi, which referred to muscles in the lower leg.
In any case, our calves comprise two major muscles: the soleus and the gastrocnemius. The gastrocnemius is the large, diamond-shaped muscles that gives our lower legs their bulge. The soleus muscle is a flat muscle that lies beneath the gastrocnemius. They taper and merge with our Achilles tendon, which inserts into our heel bone. They are responsible for the downward motion of our foot. The calf muscles pull the heel up to allow for forward motion.
Calf Strain Symptoms
The most common injury to our calf muscle is a calf strain, which is also called a pulled calf muscle and a calf muscle tear. In actuality, the two conditions refer to different degrees of the same problem. They result from overstretching the muscle and tearing some or all of the fibres. The difference is in severity.
The most severe injury is a rupture, in which the muscle is completely torn away from the bone. The least severe is a Grade 1 strain. Strains can be cumulative, resulting from injuries over time, or instantaneous, occurring as the result of a particular movement or injury.
With a Grade 1 calf strain, the muscle is partially stretched; a few fibres may be torn. The muscle may feel tender or painful, but your motion isn’t impaired and you can walk normally.
A Grade 2 calf strain is a moderate injury with more stretching and more muscle fibres torn. You may feel a snapping or pulling sensation when the tears occur and you’ll probably feel tenderness and some pain. You’ll find a loss of strength in the calf and may find yourself limping as you walk.
A Grade 3 calf strain is a severe tear of your muscle fibres; it may even be torn all the way through. This is called a rupture and the muscle itself may collapse or roll up into a ball that can be seen under the skin. You should feel extreme pain and won’t be able to walk.
Calf strains mean injured muscles and disrupted cells, leading to bleeding and bruising under the skin. Bruising may extend down the leg toward the ankle as gravity forces some of the blood lower. There will likely be swelling in the area and the muscles may feel tight.

Common Causes for a Calf Muscle Injury
Often, a calf muscle injury occurs during a sporting activity when you push off on your foot quickly to achieve a burst of speed. Athletes in sports such as tennis, baseball, soccer and track are often subject to strains, as are gymnasts and dancers.
In general, calf muscle injuries are caused by sudden or forceful, uncontrolled movement, and can occur instantly – an acute injury – or over time – an overuse injury. As we age, our calves become more vulnerable to injury.
Calf Strain Treatment
When a calf strain first occurs, take care of it during the first 24 hours by adopting the RICE method: Rest, Ice, Compression and Elevation. This includes resting on your couch, elevating your injured leg, icing it every two hours for about 20 minutes and wrapping it tightly in an elastic bandage. If you must walk, heel lifts in your shoes are recommended.
For Grade 2 or 3 strains, you’ll probably want to see your physician for an accurate diagnosis. A Grade 3 strain may require surgery to repair the tear, and you may need to undergo an MRI (magnetic resonance imaging), a CT (computed tomography) scan or a calf muscle ultrasound to confirm the diagnosis.
For Grade 1 and 2 strains, your physician will probably suggest a course of physiotherapy to help you rehabilitate your injured calf. Your physiotherapist will design a course of treatment that will encompass minimizing pain, improving motion and strength and minimizing recovery time. To minimize pain, a combination of hands-massage, ultrasound, electricity and taping may come into play.
Initially, your physiotherapist may gently manipulate your calf to allow gentle motion; you’ll progress to exercises and stretches. You’ll also start to do strengthening exercises, possibly employing weights or machines to work your calf appropriately. Your physiotherapist will work with you to achieve your goals of returning to activity and participating in the sports you love.
Any injury takes time to rehabilitate, so the best strategy is to prevent it from occuring in the first place. Be sure to do warmup exercises before participating in a sport and follow a stretching and strengthening program during the off season. Wear shoes that fit properly and don’t increase the intensity of your activity too quickly. There are no guarantees that injuries won’t happen, but these measures will make it less likely.
Let's get your calves some relief!
What is Osteoarthritis of the Hip?
With our aging population here in Canada, you may have noticed an increasing number of people walking with canes or limping as they walk. Aging translates to wear and tear on our bodies, and our joints are very susceptible.
One of the most common ailments as we age is osteoarthritis or arthritis of the bones, often called “wear and tear” arthritis. Osteoarthritis can occur in any of our joints, and the hip is one of its most common locations.
A 2009 Statistics Canada survey found that arthritis affects 10 per cent of the Canadian population ages 10 and up. Of those 20 and older, 37 per cent of arthritis sufferers said osteoarthritis was their sole arthritic condition; two per cent experienced hip pain; 29 per cent had knee pain and 29 per cent experienced both. These numbers certainly don’t prompt us to cheer, “Hip, hip, hooray!”
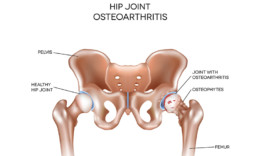
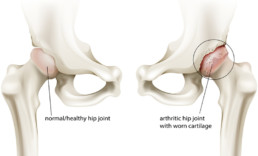
Osteoarthritis Hip Pain Explained
The hip is a ball and socket joint; the head of the upper leg bone, or femur, fits into the socket created by the acetabulum, a section of the large pelvis bone. The surfaces of both bones are generally covered with cartilage, a slippery substance that protects and cushions them. Between the bones, there is also a thin layer called the synovium, which produces fluid to lubricate the cartilage to ensure that movement happens smoothly. The cartilage also helps to absorb any shocks that aren’t dispersed by your hip bones.
With osteoarthritis, the cartilage begins to wear away and becomes rough in the process. The protective space between the two bones shrinks and, without cartilage, the bones may rub against each other. Bone spurs may also pop up, attempting to compensate for lost cartilage. It’s a slow process, but one that is increasingly painful.
Risk Factors
Although the actual cause of hip osteoarthritis and deterioration hasn’t been identified, you are more likely to suffer from it if you have one or more risk factors, including aging; heredity or congenital defects; previous trauma to the joint, such as a broken hip from years earlier or effects of sporting activities; obesity – the hip experiences six pounds of pressure for every pound we gain; and gender – women are more likely than men to experience it.
Osteoarthritis Hip Symptoms
Because hip osteoarthritis is an ailment that develops slowly, people often ignore it until it affects their daily activities. If you have hip osteoarthritis, you may have stiffness in the groin, buttocks or thigh after sitting or lying down for long periods of time, including when you arise in the morning.
You’ll will likely have pain that will worsen over time, especially when you put weight on the hip; it may radiate down the thigh to the knee. You may have some swelling, which can weaken the muscles supporting the joint. Your hip joint may lock or stick periodically and there may be a sensation of bones rubbing against each other – a crunching or popping sensation.
Walking may be painful and you may unconsciously avoid putting weight on the hip, giving your gait a limping or lurching motion. You may have some loss of function – tasks that require bending, such as tying your shoes, may become difficult, and it may be a challenge to get into a car or a chair.
Treatment for Osteoarthritis of the Hip
In addition to discussing your history and doing an examination, your doctor will test your range of motion and check for pain points. He/she may order an MRI or an X-ray to confirm the diagnosis.
It isn’t possible to reverse the damage done to your hip by osteoarthritis, but you can slow its progress and address the symptoms. Relieving pressure on the joint through weight loss and/or muscle strengthening are common approaches. For more severe cases, injections and surgery may be suggested.
Any approach to treatment should aim to reduce pain and ensuring that you can function well enough to carry on with your daily activities. You’ll need to find the proper balance between activity and rest; inaction simply exacerbates the condition. You can also use a cane in the opposite hand and/or wear cushioned shoes to relieve some of the pressure on the hip when walking.
Non-invasive treatment should be your starting point, and physiotherapy is a useful tool to strengthen your surrounding muscles, increase range of motion and reduce pain. Your physiotherapist will start by manipulating your hip, moving on to designing a course of stretching and strengthening exercises.
Osteoarthritis hip exercises can also decrease stress on the hip and increase stability. They may also help you modify your gait. You’ll want to minimize activities, such as running, that cause pain and try those, such as swimming, that don’t place stress on the hip.
More Invasive Treatments
You may also consider more invasive options. Your physician may suggest steroid injections to reduce swelling or hyaluronic acid injections that provide lubrication to the joint to make movement easier. They don’t work equally well for everyone, but if they are successful, the impact lasts anywhere from six months to a year.
Surgery is the most drastic response to hip osteoarthritis. If the osteoarthritis is having a major impact on your lifestyle, you may want to consider it. There is arthroscopic surgery that can be used to remove bone spurs or loose pieces of cartilage; osteotomy that reduces friction by aligning bones properly; and total hip replacement, which replaces your joint with an artificial one. Discuss these possibilities with your physician if the osteoarthritis becomes severe.
Finally, don’t take your condition lying down (you’ll get stiff!). Be proactive in addressing it by staying active, losing weight and adopting a course of exercise that will strengthen the muscles around the hip.
Let's get you some relief!
How to Heal a Strained Hamstring
If you work for a large organization or are required to deal with one, you may have been hamstrung – prevented from taking action – by the endless bureaucracy. But hamstrings? What are they and what’s the relation between the two words?
Hamstring vs. Hamstrung
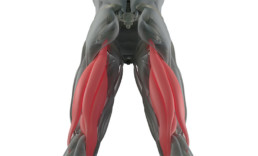
The hamstrings are the long, tendonlike muscles that run along the back of your thigh from buttocks to knee. The first syllable comes from the Old English ham or hom, meaning the hollow or bend of the knee; the strings refer to tendons. Put the syllables together and you have hamstrings: the tendons at the bend of the knee.
If you are hamstrung, technically you have been crippled by these tendons being cut; less literally however, you have been prevented from acting or being efficient.
Hamstrings Explained
Your hamstrings are crucial to your body’s motion. There are three hamstring muscles that extend from your buttocks to your knee. Your hamstring muscle group consists of the biceps femoris, the semitendonosus, and the semimembranosus. This trio of muscles is the grouping that is primarily responsible for straightening your hip and bending your knee.
What Does a Strained Hamstring Feel Like?
If your hamstring strain is a mild one, you may not even notice it until you stop exercising or until the next day when there might be tightness, soreness and bruising; however, the strength of your hamstring shouldn’t be affected.
More severe hamstring injuries include symptoms that may include a sharp, sudden pain in the back of your thigh or in your buttocks; a sensation of popping or tearing in the muscle; swelling; bruising; tenderness when touched; the inability to straighten your leg or lift it when lying down; and challenges in walking or in sitting comfortably.
With a Grade II strain, you’ll lose some leg strength and if the strain is a Grade III strain, you’ll likely be unable to use your leg.
Hamstring Injuries
Hamstring injuries generally result when the muscles come into contact with excessive force. The sudden starts and stops that athletes make while running or the cutting or jumping movements they make when playing soccer or basketball may cause a strained hamstring.
Overstretching the muscles while lifting something heavy or while hurdling or kicking can also result in injury to your hamstring group. The muscles may even become overloaded which can result in a hamstring tear. A sudden increase in the intensity of exercise or training can lead to hamstring injuries, as can running on hard surfaces, poor pelvic alignment and stress on the body due to obesity.
Hamstring strains come in three flavours, or degrees or seriousness:
- A Grade I hamstring strain (or tendinitis) is a mild overload with minimal muscle tearing involved; it will feel like a muscle pull or cramp.
- A Grade II hamstring strain is a moderate strain with partial tearing of the muscle that may be accompanied by a stinging or burning feeling at the back of your thigh.
- A Grade III hamstring strain, the most severe, is a completely torn muscle that may leave a knot or lump at the spot where the tear has happened.

Treatment for a Strained Hamstring
How to treat a strained hamstring depends on the severity of the strain. Mild strains can be treated at home, similar to any other minor sports injury. The RICE approach works well: rest, ice, compression and elevation. Avoid physical activity; apply cold packs to your hamstring for 15 to 20 minutes every few hours; use an elastic bandage to wrap and compress the thigh to reduce swelling; and keep your leg raised on pillows to further minimize swelling. You can also take over-the-counter painkillers, such as non-steroidal anti-inflammatory medicines.
If the strain is severe, surgery may be required to repair the tear. Consult with your physician if you suspect a Grade III strain.
Once the initial pain and swelling are through, you’ll undoubtedly want to return to physical activity. However, it’s wise not to rush yourself. You shouldn’t consider returning to your previous level of activity until you can move your injured leg as freely as the other leg and it feels just as strong. You shouldn’t feel pain as you walk or accelerate. Don’t push yourself; you don’t want to impair your muscle’s function permanently.
A physiotherapist can help you rehabilitate your strained hamstring. He or she can help you learn to move in a way that doesn’t put pressure on the injured area and assist you reach your movement goals. Your physiotherapist can prescribe a course of muscle strengthening exercises to focus on weak areas. He or she can also provide support through manual manipulation of areas that are difficult to reach.
Injury prevention
Those who have experienced a strained hamstring have a chance of it recurring, since the muscles have been weakened. However, everyone can take steps to prevent a hamstring injury by warming up properly before exercising; avoiding the temptation to ramp up the level of a new activity too quickly so the body has time to accustom itself; and knowing and learning proper movement techniques for both sports and lifting/moving heavy items.
Did You Injure Your Hamstring?
What is Facet Joint Syndrome?
When we think about our joints, it’s the larger ones that usually come to mind: hips, knees and shoulders, for example. We rely on them to keep us moving, but we generally don’t think about them unless they aren’t working well.
We do have other joints, however, that are equally important to our well-being, although we’re not usually aware that they exist. They are called facet joints and are located on the back of the spinal column.
Facet Joint Anatomy
Each vertebra has two facet joints, one on each side of the spine. They are the joints responsible for spine stability and flexibility and make it possible for you to bend and twist.
The facet joints in each area of the spine are angled and shaped differently in each region of the spine: cervical, lumbar and thoracic. When they are healthy, they are cushioned by cartilage, allowing them to move smoothly against each other and are lubricated by synovial fluid to prevent wear and tear.
Like any joint, your facet joints are subject to injury or pain. When these joints become painful and swell, the result is called facet joint syndrome.
The joints can also be injured; the stiffening of facet joints is called hypomobility; excessive joint motion is called hypermobility. Facet joints can also lock in place, impeding movement in the opposite direction.
Facet joint syndrome can generally be attributed to the combination of injury, excessive pressure and aging. Discs in the spine can degenerate and collapse, affecting the alignment of your facet joints. The misalignment wears on the cartilage, which is eventually destroyed, along with the lubricating synovial fluid, leaving bone rubbing on bone.
Facet joint problems are common causes for neck, back and thoracic spine pain. Generally, 55 per cent of facet joint syndrome sufferers have pain in their cervical (neck) region, while 31 per cent have problems in their lumbar (back) area.
What are Symptoms of Facet Joint Problems?
Unfortunately, facet joint inflammation can be confused with other conditions. In the cervical region, the symptoms may be similar to those of a herniated disc or a torn spine muscle. Abdominal problems and neck issues may also mimic the symptoms of facet joint issues, so a careful diagnosis is imperative.
Symptoms of facet joint problems may include:
- Acute, intermittent episodes of pain in the lumbar or cervical regions of the spine that occur a few times a month or year;
- More discomfort when leaning backward than forward;
- Low back pain that radiates through the buttocks and the back of the upper legs, but not the front of the legs or below the knees;
- Pain in the shoulders and upper back that doesn’t affect the arms or lower back; and/or
- Pain points above the facet joints and loss in spinal muscle flexibility.
If you have facet joint syndrome, you may have difficulties in bending or twisting your spine. Issues with the facet joints in your neck may make it challenging to turn your head left or right, while problems with facet joints in your back may make rising from a chair hard to accomplish. Lumbar facet joint syndrome will also make sitting and riding in a car challenging.
Diagnosing Facet Joint Syndrome
Facet joint syndrome will be diagnosed by your physician based on your symptoms, your history, an examination and tests: an X-ray, a computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan.
What Helps Facet Joint Pain?
Your physician will probably refer you to a physiotherapist to help you rehabilitate your joints, restore your range of motion and alleviate your pain.
Your physiotherapy treatment will generally include a course of exercises to restore movement, strength and flexibility, along with soft-tissue massage; acupuncture is also an to alleviate localized pain. Potentially, spinal traction and joint manipulation will also be recommended.
Your physician may also suggest non-steroidal anti-inflammatory drugs to alleviate pain quickly and prescribe muscle relaxants. If the pain continues, your physician may give you a steroid injection for temporary relief.
Prevention
Although facet joint syndrome is partially a consequence of aging, it is possible to make lifestyle choices that reduce your chance of developing it as you age. By exercising regularly, maintaining a healthy weight, eating a nutritious diet, practising good posture, and avoiding tobacco and excessive alcohol consumption, you can slow down the forces that cause it.
Suffering from Facet Joint Syndrome?
What is Post-Concussion Syndrome?
Hard hits to the head in any sport, including ice hockey and football, can cause mild traumatic brain injury, which is essentially how a concussion is defined. Violent shaking or the impact of a car crash can also lead to a concussion.
Post-Concussion Syndrome
As if an injury to the brain isn’t worrisome enough, there is also the possibility of developing post-concussion syndrome. Post-concussion syndrome refers to the persistence of various concussion symptoms long past the time of injury.
Researchers haven’t yet identified the reasons why some concussion victims suffer from post-concussion syndrome and others do not.
Some researchers believe the syndrome is caused by structural damage to the brain or disruption of the messaging system within the nerves, resulting from the impact that first resulted in a concussion. Others contend that the causes are rooted in psychological factors, since a number of the most common symptoms are also seen in people with anxiety, depression or post-traumatic stress disorder (PTSD).
Both the physiological impact of a concussion and the emotional reaction to it can contribute to post-concussion syndrome. You may be more susceptible if you have a history of PTSD, depression or anxiety, or if you have significant life stresses, poor coping skills or poor network of social supports.
How Long Can Post-Concussion Syndrome Last?
Most people who suffer concussions recover within a few months, but, for others, symptoms linger on. These varied symptoms are generally labelled as post-concussion syndrome, a poorly understood and often misdiagnosed condition that can greatly affect quality of life.
Post-Concussion Syndrome Symptoms
Post-concussion syndrome is a difficult condition to diagnose because its symptoms can often be attributed to other causes and may also be vague.
Some of the most common post-concussion syndrome symptoms are
- Headaches
- Dizziness
- Problems with sleep
Other symptoms – physical, emotional and cognitive – include:
- Irritability or aggression on little or no provocation
- Apathy or lack of spontaneity
- Changes in personality
- Difficulty finding words
- Trouble in busy environments
- Light sensitivity
- Noise sensitivity
- Nausea/vomiting
- Difficulty following conversation that includes several people
- Difficulty initiating tasks
- Persevering at tasks.
In making a diagnosis, your physician may consider your history of head injury and symptoms, conduct a physical exam and request a magnetic resonance imaging (MRI) or computed tomography (CT) scan to check for any structural abnormalities in the brain. They may also attempt to rule out other causes of the symptoms, such as bleeding in the brain or infection.
Post-Concussion Syndrome Treatment
There is no standard way of treating post-concussion syndrome. Your physician will provide and/or recommend treatment tailored to your individual symptoms. Everyone has a different mix of symptoms that occur with different frequencies. Education is a powerful tool in addressing post-concussion syndrome, because addressing the fears about the condition often help ameliorate symptoms.
If you have headaches, some of the medications used for migraines or tension headaches seem to be effective. Be aware that overuse of over-the-counter and prescription medications may lead to continuing symptoms.
For cognitive symptoms of post-concussion syndrome, time may be the best healer. Cognitive therapy may also be helpful, especially if it focuses on areas that need strengthening. Cognitive symptoms may increase with stress, so learning stress management techniques may lessen them; relaxation therapy is another option.
For cases of post-concussion syndrome that exhibit symptoms of depression or anxiety, the sufferer may opt for psychotherapy or request treatment with anti-depressants.
To improve quality of life, a course of physiotherapy may be suggested. Patients with post-concussion syndrome recover faster with physiotherapy than with rest alone, researchers have found (Schneider KJ et al. 2103). Physiotherapists may use various techniques, depending on symptoms. Manual therapy may calm the nervous system and acupuncture may improve sleep and headaches. Exercise therapy may help with balance and sensory reintegration.
Concussion Prevention
There are no guaranteed ways of preventing post-concussion syndrome, but it is possible to take precautions against suffering a concussion in the first place.
Suggestions include:
- Avoid motor vehicle collisions: drive defensively and eliminate distractions such as phone calls or eating.
- Be cautious when playing sports: wear appropriate safety gear and avoid head collisions.
- Avoid tripping and falling by keeping clear paths indoors: be careful of throw rugs, watch placement of pet dishes and be aware of loose flooring.
- Educate yourself on concussions: be aware of risk factors, signs and symptoms, and how they can affect your health.
Your brain is precious – take good care of it and don’t return to your routines until you are completely symptom-free.
Suffering From Post-Concussion Syndrome?
What Is Spinal Stenosis?
Referring in frustration, to a “pain in the neck” is a figurative way of calling someone annoying. However, it’s also an apt descriptor for cervical spinal stenosis, an ailment that literally can cause a pain in your neck – and other places, as well.
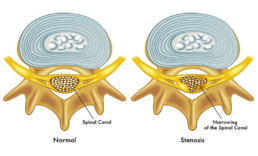
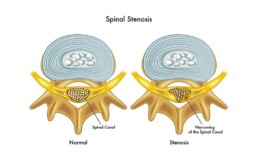
Definition
Spinal stenosis refers to the narrowing of the spinal canal, which houses the spinal cord, and the openings in it that provide passage for peripheral nerves that thread their way to other parts of the body. This narrowing can choke the spinal cord and/or the roots of your nerves.
There are two types: cervical spinal stenosis, which affects the spinal column in the neck region, and lumbar spinal stenosis, which narrows the spinal column in the lower back.
What Causes Spinal Stenosis?
Aging is the most prevalent cause of spinal stenosis. As you age, your spine gradually degenerates. The discs between your vertebrae lose height through dehydration; your bones and joints may enlarge due to increased stress on them and destruction of cartilage, potentially leading to bone spurs that occupy space in the spinal canal; and your ligaments may thicken and calcify, encroaching on the space in the nearby canal.
Middle-aged and elderly people are also subject to osteoarthritis of the spine, or spondylosis, which is chronic and the result of wear and tear on the spine. It can also lead to the formation of bone spurs that constrict the spinal canal and cause spinal stenosis.
Although people over the age of 50 are the most likely to suffer from it, younger people who suffer a spinal injury or are born with a narrow spinal canal are also subject to spinal stenosis.
What Are the Symptoms of Spinal Stenosis?
Spinal stenosis may be present without your being aware of it. The spinal canals of many people over 50 narrow, but it only becomes apparent when the nerves are squeezed and they feel the resulting symptoms. It may take time for the symptoms to develop.
Your family physician will generally be able to diagnose spinal stenosis based on your symptoms and your medical history, using appropriate tests to confirm the diagnosis. The doctor may order a magnetic resonance imaging test (MRI), X-rays or computed tomography (CT) scans to rule out other possible causes of the pain.
What Is Cervical Spinal Stenosis?
With cervical spinal stenosis, you may feel some stiffness, pain, numbness or weakening in your hands, shoulders, neck or legs. You may find that you have problems with co-ordination and balance, causing you to stumble when moving or shuffle as you walk. There may be problems with fine-motor skills, such as typing or buttoning a shirt. You may also experience some incontinence.
What Is Lumbar Spinal Stenosis?
If you have lumbar spinal stenosis, leg pain when you’re in motion will usually be your primary symptom, since the nerves in the lower spine extend into the legs. It is often more severe when your spine is extended: for instance, when you are standing straight or leaning backward. The pain generally eases when your spine is flexed: whenever you are sitting, riding a bicycle or bending over your shopping cart.
Lumbar stenosis also manifests itself through additional symptoms, including low back pain; cramping, weakness or numbness in the legs, feet or buttocks; thigh and leg stiffness; and possible loss of bowel or bladder control.
What Is the Best Treatment for Spinal Stenosis?
Once a diagnosis is made, your physician will probably suggest physiotherapy as a treatment option that will ease the symptoms. In extreme cases, surgery is warranted to relieve pressure on the spinal cord and nerves, but, usually, you can address the symptoms through other means.
At home, you can use non-steroidal anti-inflammatory drugs to ease the pain and reduce the inflammation. Your physiotherapist will do the same for you, using methods that may include ice, unloading taping techniques, electrotherapy, soft tissue massage and acupuncture.
Spinal Stenosis Exercises
Once the inflammation settles, your physiotherapist will help you focus on range-of-motion and alignment exercises, as well as muscle strengthening.
Exercises will usually take the form of lower abdominal and core stability exercises, since you want to strengthen the muscles that control and stabilize the movement of your spine.
Cervical spinal stenosis exercises will aim to maintain flexibility and strength and improve posture.
Prevention
There are some basic things you can do in order to prevent symptoms to manifest themselves or recur:
- Maintain a healthy body weight.
- Develop or maintain good posture.
- Exercise regularly, including stretching exercises, such as yoga.
- Don’t smoke, since smoking decreases bone density and increases risks of fracture and bone deterioration. It has also been linked to disc problems.
Spinal stenosis should be taken seriously; if you follow the guidance and treatment plan you receive, you usually should be able to make your pain disappear within a reasonable timeframe.
Let’s Get You Some Relief!
What is Sciatica?
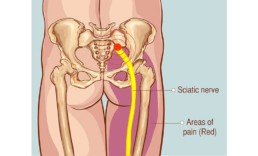
Do you have pain radiating from your buttock to your calf? Perhaps you have discomfort running from groin to knee. Interestingly, both of these diverse problems may fall under the rubric of sciatica. So, what is sciatica and what causes sciatic nerve pain?
Sciatica Pain
Sciatica is not actually a medical diagnosis; it is a term that refers to any type of pain or weakness that is caused by irritation or injury to your sciatic nerve. Sciatica pain is most prevalent among people 30- to 50-years old.
The sciatic nerve is the longest nerve in the body. It comprises a number of nerves that exit your lower spine and meet up. The sciatic nerve runs from your lower back through the buttocks and hamstrings into your lower leg.
Sciatica Symptoms
Sciatica manifests itself in a number of ways, usually occurring only on one side of the lower body. Some of the most common sciatica symptoms are:
- Weakness or numbness in moving your foot or leg.
- Constant pain in the rear calf.
- A tingling or burning sensation in the leg.
- A “pins and needles” sensation in the leg.
- Shooting pain in the leg, making walking or standing up a challenge.
- Constant pain in the buttock that may radiate down the leg.
- Pain that decreases when walking or lying down, but ramps us while sitting or standing.
Your sciatica symptoms may intensify when you sneeze, cough or make other sudden movements or when you change positions.
Sciatica Causes
There are six injuries that are most often implicated in sciatica:
- Degenerative disc disease. Although our discs normally degenerate a bit with age, the weakened discs in some bodies irritate the nerve root, causing sciatica. Disc degeneration may also lead to bone spurs, which may press against a nerve and result in sciatica.
- Lumbar spinal stenosis. A narrowing of the spinal canal is relatively common in adults older than 60 and can cause pressure on the sciatic nerve through one or more factors, including bulging discs, overgrown soft tissue and enlarged facet joints. Spinal arthritis often accompanies spinal stenosis and can contribute to sciatica.
- Herniated lumbar disc. Herniated discs result when the fluid inside the disc leaks out beyond the core and irritates the nearby nerves, causing sciatica.
- Sacroiliac joint dysfunction. The sacroiliac joint is located at the base of the spine, and anytime it is irritated, the nerve that lies on top of it is also subject to irritation, causing leg pain similar to sciatic pain.
- Piriformis syndrome. The sciatic nerve runs under the piriformis muscle in the buttocks and may be subject to irritation or pinching by the muscle, causing sciatica-like pain.
- Isthmic spondylolisthesis. A small stress fracture in a vertebra can cause the vertebra to slip forward onto another, collapsing disc space and pinching the sciatic nerve.
Sciatic Nerve Pain Treatment
In order to treat sciatic nerve pain, your physician or physiotherapist must determine the underlying problem that is causing it. This can be a challenge, since two cases of sciatica can easily have the same symptoms but different causes. You may need an X-ray, a CT scan or an MRI to assess potential problems with your vertebrae.
Once this is accomplished, the focus can shift to relieving pain and pressure on the sciatic nerve and restoring the range of motion:
- Ice. Icing the affected area can help to reduce inflammation. Ice should be wrapped in a towel and applied for 20 minutes at a time.
- NSAIDs. Non-steroidal anti-inflammatory medications such as ibuprofen help to reduce the inflammation that may be a source of irritation for the sciatic nerve and surrounding tissues.
- Physiotherapy. Your physiotherapist will prescribe a course of stretching exercises to loosen any muscles that may be placing pressure on the sciatic nerve, as well as joints and tendons, plus strengthening exercises to help prevent a recurrence of the pain. Physiotherapy treatment for sciatic nerve pain may also include:
- Massage therapy to increase blood circulation and release of endorphins to fight pain
- Trigger point therapy
- Spinal mobilization
- Ultrasound and electrical stimulation
- Acupuncture. Long recognized for its effectiveness in relieving back pain.
How to Prevent Sciatic Nerve Pain
Unfortunately, sciatica has a tendency to re-occur, and bouts of sciatica can last as long as six weeks. You can play a part in preventing an episode of sciatica by playing an active role in your own physical health:
- Regular exercise. Make exercise part of your routine, focusing on activities or routines that strengthen the back and abdominal muscles. Swimming and Pilates are ideal; ask your physiotherapist about individual exercises.
- Posture. Keep an eye on your posture when sitting and standing. You may want to request an ergonomic assessment at work to ensure your chair, computer and desk are arranged to minimize inappropriate stresses.
- Sleep posture. Consider sleeping with a pillow between your knees or at your side so that your back is supported.
- Movement. If you have a desk job, make sure to get up and move every 20 to 30 minutes. Walk to the photocopier, the coffee pot or just up and down the hall.
- Lifting. Be sure that you lift heavy objects by using your leg and hip strength.
Sciatica is unpleasant, but the pain can be addressed. Treatment that occurs during the first 48 hours of onset will shorten the time you are indisposed.
Let’s Get You Some Relief!
What is Temporomandibular Joint Disorder (TMJ)?
Here’s a topic worth jawing about: temporomandibular joint disorder, or TMJ disorder (TMD), a facial joint disorder that is painful, rather than fatal; however, it can be uncomfortable.
When people who suffer from TMD open their jaws, the movement may provide “musical” accompaniment in the form of clicks or popping sounds that they are unable to prevent. But what is TMJ?
TMJ Disorder (TMD)
The temporomandibular joints are the joints connecting the temporal bones of the skull to the mandible, or jaw bone, hence the name. It is commonly referred to as the TMJ. There is one on each side of our heads.
These joints, which are lined by cartilage and contain a fibrogelatinous disc between the bones, open and close like hinges. They allow the jaw to move both up and down and side to side, making them among the most complicated of the body’s joints.
A TMJ disorder refers to problems with the jaw joints, muscles or fibrous tissues that connect them. TMJ disorders are most prevalent among women in their early 20s or during their 40s and 50s, while undergoing menopause. Men are affected by TMD less frequently.
TMJ Symptoms
Common TMJ symptoms include:
- Pain. Pain while moving the jaw is an obvious symptom of TMJ disorder, but the disorder may also cause headaches or migraines, earaches, neck aches and back aches. The earaches may be accompanied by ringing or buzzing your ears. Your chewing muscles will generally be tender and painful when touched.
- Minimal movement. Limited movement may prevent you from fully opening your mouth or from moving your jaw in particular directions. For example, non-sufferers can generally hold their index, middle and ring fingers horizontally and insert them easily between the upper and lower teeth. People with TMJ disorders will generally find it difficult to open their mouths so wide.
- Noise pollution. TMJ disorders are often accompanied by sounds that occur when you talk, eat or open your mouth. The noises may be clicking, popping or grinding sounds and will be present concurrently with the pain or restricted movement. If the noises are not linked to one of the other symptoms, they are generally harmless.

Diagnosis
A TMJ disorder will generally be diagnosed by a doctor or a dentist based on a physical examination in combination with a review of the patient’s medical history. Depending on the outcome, a magnetic resonance imaging (MRI) test for your disc, an X-Ray of your teeth or a Computed Tomography (CT) scan of your bones may be required.
What Is the Best Treatment for TMJ?
You may be able to treat mild or moderate TMJ disorder at home by making lifestyle changes. TMJ home treatment may involve a reduction in joint movements and more rest for the jaw by avoiding chewing gum and tensing the jaw and by eating only soft foods. The application of ice or moist heat may also be useful, along with non-steroidal anti-inflammatory drugs.
Reducing stress in your life may also be helpful; yoga and meditation are often good ways to alleviate stress, and counselling (therapy) can be useful, too. You may also wish to try biofeedback or acupuncture to help relieve pain.
Is There Physical Therapy for TMJ?
A visit to your physiotherapist is recommended if symptoms are not relieved with home treatment and are related to muscle tension. Your physiotherapist can prescribe a program for you that includes learning and practicing techniques for regaining normal jaw movement.
TMJ exercises may relieve pain, reduce tension and strengthen the jaw area in order to prevent future flare-ups. Your physiotherapist will be able to recommend an appropriate series of exercises that begins with massaging the area to reduce tension and pain. You’ll move on to relaxation, strengthening and stretching exercises. They may also use ultrasound treatments.
If none of these approaches proves effective, your physician or dentist may suggest a corticosteroid injection, arthroscopy or open joint surgery.
Remember: pain is your body’s signal that something isn’t right. If your jaw begins to ache regularly, don’t ignore the feeling. The sooner you obtain treatment, the sooner you’ll feel like yourself again.
Let’s Get You Some Relief!
What is Carpal Tunnel Syndrome?
On a daily basis, we don’t give much thought to our wrists, unless we are putting on a bracelet, affixing cufflinks or buttoning a sleeve. They are simply connectors, bringing more important body parts – hands and arms – together so they can do their work.
We do sit up and take notice, however, if those wrists begin to hurt. It’s only then that we realize how important they are to the smooth functioning of our upper extremities and how frustrating it can be when they aren’t working properly. Carpal tunnel syndrome (CTS) is a common reason for wrist pain, so it’s worth examining in more detail.
Carpal Tunnel Syndrome Explained
Carpal tunnel syndrome results from the compression of the meridian nerve, a nerve on the palm side of the wrist. The meridian nerve is located in a “tunnel” created by a wrist ligament and the carpal, or wrist, bones. The tunnel, which is about the width of a thumb, is also crowded with the tendons that allow us to bend our fingers. Compression is generally caused by pressure on the nerve due to crowding or irritation.
What Causes Carpal Tunnel?
A frequent culprit is continued finger use, especially in situations that include vibration, and extreme wrist positions can contribute to CTS, as can repetitive motion. In today’s technology-focused world, we tend to associate CTS with working at a keyboard all day, but people working on assembly lines are three times more likely to develop it.
Other conditions that may lead to carpal tunnel syndrome, include:
- Wrist injuries, such a sprains and fractures;
- Swelling and inflammation of the wrist tendons;
- Metabolic or hormonal changes, including pregnancy, menopause and thyroid imbalance;
- Scar tissue from repeated traumas;
- Degenerative or rheumatoid arthritis: and
- Diabetes.

Prevention: Minimizing Stress to Hands and Wrists
There is no surefire way to prevent carpal tunnel syndrome, but there are actions you can take to minimize the stress to which you subject your hands and wrists as an attempt to keep it from developing:
- May the force NOT be with you. Reduce the amount of force you use when doing work with your hands; most of us apply more than is necessary. For writing, use soft-grip implements.
- Ergo, it’s ergonomic. Have your work station assessed from an ergonomic point of view to ensure that is suited to your height, posture and work you do.
- Wrist readjustment. At a keyboard, keep your wrists extended, rather than flexed upward or downward to ensure that you don’t put undue strain on your nerves and tendons.
- Perfect your posture. Keeping your torso, neck and shoulders aligned can help ensure that you position your hands and wrists properly.
- Create warmth. Hand pain and stiffness happen more easily in the cold, so keep your work environment warm. If you can’t adjust the temperature, wear gloves to warm your hands and wrists.
- To your health. Overall good health is important to keeping diseases that may lead to carpal tunnel syndrome at bay, so take good care of yourself.
Signs and Symptoms of Carpal Tunnel Syndrome
So, what does carpal tunnel feel like? If you experience any of the following, they may be signs that you are suffering from carpal tunnel syndrome:
- Pins and needles that affect the thumb and first two fingers;
- Numbness in the wrists or fingers;
- A clumsy feeling in the affected hand; or
- Weakness of the hand or in grip strength.
You may notice the feelings more clearly at night and may be awakened by the pain.
Diagnosing Carpal Tunnel Syndrome
Oftentimes, your physician or your physiotherapist can diagnose CTS without much trouble if you have the standard carpal tunnel symptoms, but there are also some tests that can be used to confirm its presence, including:
- Finger and thumb grip strength testing;
- Wrist and hand range of motion testing;
- Reflex hammer testing; and
- Electrical studies showing nerve transmission.

How to Treat Carpal Tunnel
Carpal tunnel syndrome doesn’t require surgery, except in the most extreme cases. Initially, your physician will suggest physiotherapy as a carpal tunnel treatment. There are a number of simple carpal tunnel exercises that can relieve the pain and strengthen the wrist to prevent a recurrence of CTS.
Depending on the severity of the compression and inflammation, your physician may suggest wearing a resting wrist brace at night to prevent your wrist from assuming an injurious position and/or a working wrist splint to wear during the day. A steroid injection may reduce inflammation and its effects may last for weeks or longer.
Carpal tunnel syndrome is a minor injury with major consequences for our daily routines. It’s wise to take action as soon as symptoms appear so that the injury doesn’t progress. Ice the affected area and take frequent work breaks, and seek treatment if it continues.
Let's get you some relief!
Laser Therapy for Pain
“No pain, no gain,” says the common saying, but those who are victims of physical pain would undoubtedly agree that this aphorism refers to growth and emotional pain. Physical pain, by contrast, is a hindrance to growth.
When you are hemmed in by pain, your options become more limited; you are unable or unwilling to use your body in many of the ways you once took for granted. It’s a frustrating feeling and you are keen to explore all options for banishing that pain and expanding your opportunities. And that’s where laser therapy enters the picture.
What is Laser Therapy?
Laser therapy is a non-invasive method of treatment that relies on light beams of various wavelengths delivered by a laser to reduce pain. It helps to heal soft tissue and provides pain relief.
Laser therapy relies on the laser, a device based on a theory first proposed by Albert Einstein in 1916, the Theory of Light Amplification through Stimulated Emission of Radiation (LASER).
Hungarian physicist Andre Mester was the pioneer in using a low-powered laser for medical treatment, beginning in 1967, only a few years after the first working laser was produced.
How Does It Work?
Laser light on the infrared spectrum interacts with the body’s tissues, generally absorbed by the skin through a handheld laser device that targets a specific area. The light emitted by the laser creates physical changes in the cells in a process called photobiomodulation.
It passes through the layers of skin and interacts with the light-sensitive elements in a cell, increasing internal metabolic activity and increasing the flow of nutrients across the cell’s membrane.
In other words, the laser brings light to living tissues and its energy increases circulation, which in turn brings nutrients and water to the cells to create an ideal healing environment for pain and inflammation reduction, stiffness and muscle spasms.
What Are the Benefits of Laser Therapy?
The benefits of laser therapy are many and varied, extending beyond pain relief:
- Acceleration in tissue repair and healing.
- Analgesia (reduction of pain).
- Angiogenesis (new vascular supply formation).
- Improved nerve function Inflammation reduction.
- Increased cellular metabolic activity.
- Reduction in fibrous tissue (scar tissue) formation.
- Stimulation of acupuncture points and meridians.
- Stimulation of immune cell activity.
In addition, there are clinical benefits. Laser therapy can offer an alternative to surgery in many cases: it’s non-invasive, it can be effective for conditions that are difficult to treat using more traditional methods, it’s easy and, it is backed by scientific proof of its effectiveness. Numerous research studies have been undertaken to illustrate the success of laser therapy.

Conditions That Benefit From Laser Therapy
Laser therapy can have a beneficial effect on a variety of conditions that involve muscles, tendons and ligaments, including:
- Low back pain
- Neck pain
- Arthritis pain
- Plantar fasciitis
- Tendonitis
- Carpal tunnel syndrome
- Fibromyalgia pain
Laser therapy can reduce healing time, thanks to an increase in intercellular metabolism. Generally, the sooner it is employed after injury or after pain becomes intolerable, the better the healing and the more quickly the pain dissipates and the healing takes place.
The more chronic the condition, the slower it may be to respond to laser therapy. The treatment is cumulative, so the patient generally needs a series of treatments to eliminate pain and promote healing.
Undergoing Laser Therapy for Pain
When you decide upon laser therapy for pain, you’ll have an initial consultation with the clinician who delivers the therapy, whether a physician, physiotherapist or other healthcare professional, to determine the extent of your injury or condition.
Treatment will follow. There is no reason to be fearful of the experience. It is painless. Treatments usually last for 5 to 20 minutes, depending on the acuteness of the injury and the size and depth of the affected area, since these high-powered lasers can deliver energy quickly.
You can expect the practitioner to use a handheld device about the size of a flashlight that he or she will run over the skin above the affected area. The laser often has changeable heads that are geared toward effectiveness in various areas of the body.
Often, you will feel a soothing, warming sensation as the photons of light pass through the skin. When the practitioner attaches a massage ball head to the laser, patients often compare the experience to a massage.
In Conclusion
In a number of provinces, including British Columbia and Ontario, laser therapy is covered by provincial healthcare plans, making it easy to choose. Given the ease of treatment and its beneficial effects, why not give Laser Therapy a try?
Let’s Ease Your Pain!
What is Intramuscular Stimulation (IMS)?
You’re in pain and the sensation just won’t go away. You may have had an X-ray or an MRI that has not discovered any problem, but the pain continues to linger. You are at your wits’ end, worrying that your quality of life will never improve, when someone recommends that you explore intramuscular stimulation (IMS). What, you wonder, is that?
What Is IMS Therapy?
IMS, or intramuscular stimulation, is a treatment for acute or chronic pain with a neuropathic (nerve) origin. It relies on the insertion of acupuncture needles, either into tender muscles or at sites near the spine where a nerve root may have become extremely sensitive.
It targets muscles that have become shortened (distressed). These spots can be problem points in the body, because contracted muscles don’t always heal properly and they press on the nerves and irritate them.
IMS therapy helps the muscles to relax and the healing process to begin. In other words, it treats the root causes of the pain you are experiencing.
Why the Pain?
Pain that occurs when there isn’t any obvious sign of tissue damage or inflammation can be perplexing and frustrating. If you can’t identify a cause, how can you obtain treatment?
Neuropathic pain generally occurs when nerves malfunction after a minor irritation. They become very sensitive and their innocent signals are misinterpreted by the brain as pain.
IMS Treatment Explained
During your IMS treatment, a physiotherapist or other trained practitioner will insert acupuncture needles into the affected muscles. Insertion of an ultra-fine acupuncture needle into a healthy muscle is painless. However, when a needle enters a shortened muscle, it grasps the needle, and this can result in a cramping sensation. This action has a threefold impact:
- It stimulates a stretch receptor in the muscle, causing it to lengthen (relax).
- It causes a tiny injury that draws blood to the area, stimulating the natural healing process; the blood contains a Platelet Derived Growth Factor to promote healing.
- The stimulation causes electrical potential in the muscle, allowing it to return to functioning normally.
An IMS treatment has very few side effects and the relief is lasting.

When Is Intramuscular Stimulation Used?
Intramuscular Stimulation is generally used for soft tissue pain when there is no sign of tissue damage or inflammation, but the pain persists. It is employed for various types of neck and back pain, frozen shoulder, tennis elbow and fibromyalgia, as well as other complaints.
It is useful in cases where the injury is too deep for other types of treatment to reach, such as pain in the pelvic area.
How Often Do You Need IMS Therapy?
The impact of IMS therapy is cumulative. After each IMS therapy session with your physiotherapist, the muscle heals a bit. Eventually, the muscle shortens and the pain dissolves. Most patients have IMS sessions weekly, but some prefer to come every other week to provide a longer recovery period.
The number of IMS treatments required is based on:
- The type of injury.
- The duration and extent of the pain.
- Whether the injury is recent.
- The amount of scar tissue that has accumulated.
What Are the Origins of Intramuscular Stimulation?
Intramuscular Stimulation originated in Vancouver in the 1970s, developed by Dr. Chan Gunn, a physician who was then working at the Workers Compensation Board. Dr. Gunn saw numerous patients whose conditions refused to respond to traditional treatment and began investigating the reasons for unresponsiveness and the potential solutions.
Intramuscular stimulation and is an anatomy specific form of acupuncture performed by specially trained physiotherapists. Although it is similar to acupuncture, IMS practitioners don’t insert needles into meridians of the body. Instead, after a medical examination, the patient visits an IMS practitioner who inserts needles based on the diagnosis.
Post-Therapy
Once your IMS treatments have dealt with your pain, you may want to talk with your physiotherapist about ways to ensure that you don’t injure your muscles and nerves again in the same way. Movement retraining can help you learn to erase any bad movement habits you have developed. Poor habits can be the result of:
- Asymmetry in movement developed at work or during recreational activities; or
- Previous injuries.
Your physiotherapist can help you assess which muscles you tighten unnecessarily and which movements you make poorly. Once you are able to recognize these weaknesses, you can practise not tightening these muscles automatically and learn to activate other muscles to balance your responses.
Movement retraining of this nature can help your body accomplish various tasks better, including sitting in a chair, squatting to retrieve something from the floor or unleashing your golf swing.
There’s No Need to Suffer Endlessly With Chronic Pain. Explore the Possibilities of IMS Therapy.
Stiff Neck Remedies
Anyone who has ever had a stiff neck knows that they’re painful and awkward. The inability to turn your head sideways without pain makes everyday tasks challenging and driving a car impossible. It’s an inconvenience that no one wants, but trying to find a stiff neck remedy is a step in the right direction.
How to Get Rid of a Stiff Neck
A stiff neck usually refers to soreness and difficulty in moving the neck side to side. In fact, it may require that you turn your entire body to look over your shoulder. The pain may be accompanied by a headache, shoulder pain or arm pain.
If a stiff neck is bothering you, try simple remedies to start your stiff neck treatment:
- Ice is nice. Apply ice to the affected area for the first 48 to 72 hours; afterward, substitute heat in the form of hot showers, compresses or a heating pad. Don’t place ice packs or heating pads next to bare skin.
- The bottle. Of over-the-counter pain relievers, that is. Acetaminophen or ibuprofen should banish the pain.
- Move it. Motion will help keep inflammation at bay, but no jerky movements allowed.
- Rub-a-dub-dub. Ask a partner or a friend to gently massage the area.
- Stiff neck exercises. Range of motion exercises gently stretch neck muscles. You may wish to consult a physiotherapist for additional suggestions.
- Chuck the cushion. Try sleeping pillowless or with a special neck pillow.
Depending on the cause of your stiff neck, some lifestyle adjustments may be in order: - Redecorate. Be sure that your work station is set up ergonomically to keep your head, neck and back in a natural position. You may need a different chair or an adjustment to the height of your computer monitor.
- Stare at the ceiling. If your sleep position is causing a stiff neck, you’ll need to modify it. Sleeping on your back or your side are best for the neck. If you sleep on your stomach, your head generally twists in one direction for hours at a time.
- Pillow talk. Buy a pillow that isn’t too high for you or too firm.
- S-t-r-e-t-c-h. You may need to stretch regularly to prevent your neck muscles from injury. A physiotherapist can design a targeted exercise program for you.

Stiff Neck Causes
To figure out how to get rid of your stiff neck, you need to look into what causes a stiff neck. The most common cause is a muscle or soft tissue sprain. The cervical spine housed in the neck comprises seven vertebrae that protect the spinal cord while connecting the skull to the upper back and its thoracic vertebrae.
To the back and side of the neck is the levator scapulae muscle that connects the neck to the shoulder, and it is this muscle that is most susceptible to sprains.
A levator scapulae strain has a variety of potential causes:
- A fall or sudden impact that moves the head side to side.
- Sleeping with the neck in an unusual position.
- Holding the head at an unnatural angle for long periods of time – for example, by cradling a phone between ear and shoulder or by looking down at a computer monitor.
- Poor posture.
- Stress or anxiety.
- An activity that requires you to repeatedly move your head from side to side, such as swimming the crawl stroke.
If the pain appears shortly after a fall, the cause will be obvious. Otherwise, you may not be able to pinpoint the exact cause; misusing your muscles over time can have a cumulative effect.
In addition, there are spine disorders that can result in a stiff neck, including:
- Cervical osteoarthritis. The breakdown of joints between the bones of the vertebrae.
- Cervical herniated disc. Breakdown of a disc’s outer layer causes fluid to leak out and cause inflammation and compression in surrounding tissues.
- Cervical degenerative disc disease. Discs lose height and hydration over time, potentially exerting pressure on nearby soft tissues, joints and nerves.
Generally, a stiff neck resulting from muscle strain should clear up on its own within a week. If the pain and stiffness remain, however, it’s time to consult a physician to determine if a spinal disorder is the underlying cause.
If your neck pain persists longer than a week, it’s possible that you have an underlying condition that is causing the stiff neck, such as those mentioned above. You should check with your physician to be sure that any serious problem is identified quickly so you can seek additional treatment. Meanwhile, heads up!
Wondering How to Fix a Stiff Neck?
Extended Health Benefits Explained
Canadians are fortunate, compared to their neighbours south of the border, in having most of our basic medical needs taken care of by the government. Of course, we do pay for health insurance in taxes – and through monthly payments for residents of British Columbia and Alberta – but we don’t panic or hesitate due to cost when we need to see the doctor. It’s a sound long-term government strategy for keeping us healthier overall.
Unfortunately, the government doesn’t fully cover all of our medical needs. Provincial health insurance generally pays 70 per cent of hospitalization costs, for example, and we need to ante up the other 30 per cent. That’s where extended health benefits enter the picture. If you’re lucky enough to work for an employer with an extended health care plan – a plan that pays for services not covered by the government – your additional benefits help close this gap.
Extended Health Insurance BC
Extended health care plans offer a variety of benefits, generally including dental care, eyeglasses, physiotherapy and massage therapy. The benefits vary from province to province: extended health insurance BC includes reimbursement for visits to naturopathic doctors, for example.
Plan members may be assigned a set dollar amount annually for each of these services; extended health benefits BC may pay a percentage of the cost of an individual service; or they may be provided with a health care savings account and allowed to allocate the annual dollars as they see fit. Depending on the service, the funds may not kick in until the plan member has spent a set amount, or deductible, on additional healthcare services.
As an employee, you may not realize the worth of extended health benefits – unless you have worked in a field where the employer doesn’t offer them. Self-employed people, too, must pay for extended health insurance out of their own pockets or pay for the entire cost of such services. These plans are a valuable part of your overall compensation package, along with sick days and vacation time. Don’t disparage their significance – and make sure to use them!
Understanding your Extended Health Care plan
Are you even aware of the scope of your extended health care? Make it a ritual to review your extended health benefits annually to see what is available. If you don’t know, you certainly can’t take advantage of them. Note each benefit, the dollar limit available and the percentage you’ll need to pay out of pocket. Some plans cover only a percentage of certain services; others may cover more once your deductible is reached.
You may also need a prescription from your physician to take advantages of some of the services. If so, you can plan ahead; when you go for an annual checkup with your family doctor, you can request prescriptions for services you plan to use sooner, rather than later.
Using your Extended Health Benefits before they expire
Extended health benefits, like coupons, have an expiration date. They generally run for a year, whether a calendar year or a fiscal year. Once the year is over, the slate of available benefits is wiped clean and the next year’s benefits are made available. Even though you may not have used all of the benefits, you can’t carry them over from year to year.
If you had a voucher for a free flight to Hawaii that was only valid until the end of the year, would you let it expire? Unlikely! Or a coupon that gives you half-price admission to Grouse Mountain and a day of skiing? Of course not. So, why would you pass up the chance to take advantage of the full range of health benefits offered to you, especially if they can improve your health?

Physiotherapy and your Extended Health Care Plan
Many of the benefits covered by extended health care plans are also preventive services, such as physiotherapy and massage. They may not be items that immediately spring to mind, unless you are in pain. However, they aren’t tailored solely for people who are suffering, and it makes sense to take advantage of them to improve your health.
Will you fall apart if you don’t go to see a physiotherapist or get a massage? Perhaps not, but why wouldn’t you access a massage or physiotherapy that will undoubtedly improve your health and prevent problems from stress or poor posture? Many extended health insurance plan providers even allow for direct billing, which means that your physiotherapist can bill them for your services directly! So, don’t procrastinate.
After reading this column, ascertain the best-before date of your annual extended health insurance plan and list your benefits. Even if they are available on a calendar-year basis, you still have more than a month until year’s end. Why not enjoy the opportunity to tune up your body and make sure it’s operating at its peak?
Ready to review your Extended Health Benefits?
What Is Kinesiology?
Many people get referred to a Kinesiologist for rehabilitation and recovery, after a motor vehicle accident or work related injury, or as part of a return to work program. Most people know what to expect from a Physiotherapist and Massage Therapist, however, many are unfamiliar with Kinesiologists and are wondering “What is Kinesiology?”.
Kinesiology Definition
Kinesiology is the multi-disciplinary scientific study of human movement, performance and function that explores the physiological, biomechanical and psychological mechanisms of movement. It considers the impact physical activity has on health, society and the quality of life.
What Is a Kinesiologist?
Kinesiologists are university-educated health professionals who seek to enhance the quality of life for patients by applying principles of anatomy, physiology, biomechanics and psychomotor behaviour to improve their functioning, performance and health. They evaluate physical issues and recommend solutions, helping patients to achieve health and wellness goals.
Practically speaking, kinesiologists employ evidence-based research in combination with assessment to assist human performance and prevent or rehabilitate injuries and other physiological problems.
Kinesiologists work in a variety of settings, including clinics and industry, and serve a wide range of clients, including professional or amateur athletes and senior citizens. They can help you with injury prevention, assessment and rehabilitation; treatment of chronic diseases; and preventative maintenance of your body.
What Can a Kinesiologists Do for Me?

Let’s take a closer look at the various services that Kinesiologist offer:
- Assessment and Active Rehabilitation. Whether you are injured in a car crash, at work or while playing soccer, a kinesiologist can help you through active rehabilitation. He or she will assess your physical function and craft a structured exercise program tailored to your individual situation that will allow you to return safely to your usual activities. People who have experienced heart attacks, strokes or traumatic brain injuries are ideal candidates for working with a kinesiologist.
- Ergonomics and Workplace Design. In the workplace, kinesiologists analyze the physical demands of specific jobs, evaluating the risk for musculoskeletal injury. They assess risk factors and adapt workplace conditions to minimize injury potential, including modifying or designing equipment and tools. They also help companies whose employees perform physical labour, kinesiologists often conduct education sessions discussing the proper postures for lifting, carrying and similar tasks as a way of preventing workplace injuries. They also design on-the-job warmup and stretching routines and may serve as coaches/supervisors for employees returning to work after injury or illness, ensuring they are properly integrated back into the workplace.
- Exercise Therapy. Their keen understanding of the mechanics of the human body makes kinesiologists ideal for helping design exercise regimens for people living with chronic diseases such as diabetes, arthritis and multiple sclerosis.
- Sport Conditioning/High Performance Training. Who better to help athletes reach their peak performance than professionals who study the intricacies of motion? Kinesiologists can assist athletes of all stripes in improving their performance, whether they are Olympic swimmers trying to shave seconds off their best times or teenage hoping for a spot on the school team. Look to them to develop well-rounded programs that encompass sport-specific skills and overall fitness. With their help, athletes can expect to improve speed, power and agility.
Kinesiology in Canada: Colleges and Associations
Twenty-three of the 38 Canadian universities from coast to coast incorporate the term kinesiology into their faculty/department names or degree designations. Provinces have professional associations that represent and advocate for their members and develop scopes of practice for their members. In BC, the British Columbia Association of Kinesiologists or “BCAK” was incorporated in 1991.

Practising Kinesiologists: Requirements in BC
Practising Kinesiologists in BC are required to have a minimum 4-year degree in specialized kinesiology or human kinetics program from a recognized post-secondary institution. They are required to commit to ongoing yearly professional development and continuing education. Here are some of the skills kinesiologists bring to the table in assessing patients:
- A thorough knowledge of the indications and contraindications to exercise;
- A thorough knowledge regarding the design and implementation of safe and effective exercise prescriptions for healthy individuals;
- A comprehensive knowledge regarding the design and implementation of safe and effective exercise prescriptions for patients with chronic disease, functional limitations, and disabilities;
- A clear understanding of the influence of commonly used medications on the response to exercise;
- In-depth knowledge of acute and chronic responses and adaptations to exercise in healthy and clinical populations;
- An ability to determine when to terminate exercise testing or training; and
- A critical understanding of diagnostic stress testing protocols and procedures.
Now that you have a better understanding of this emerging discipline, don’t hesitate to call upon a practising kinesiologist to assist you in evaluating your current fitness, helping you to reach your athletic potential or restoring your mobility after injury or disease strike.
Meet Our Kinesiologist
What Is a High Ankle Sprain?
If you’re a professional basketball fan you’ve undoubtedly seen one of the players on your favourite team hobbling off the court in pain, often supported by teammates or the trainer. If the player is suffering from a high ankle sprain, he could be off the court for as little as a week for a mild sprain, but the more serious version could keep him out for months. When a star player gets injured in this fashion, he may not break the ankle, but he breaks many fans’ hearts.
How Does a High Ankle Sprain Occur?
A high ankle sprain differs from the mild sprain that occurs when you roll your ankle. The ankle joint is a complex one, because it is the location where the two lower leg bones, the tibia (shin bone) and the fibula (outer leg bone), come together and join to the foot.
A high ankle sprain is an injury
- to the ligaments (connective tissue that joins two bones),
- of your sydesmosis (a fibrous joint at the juncture of the two leg bones just above the ankle bone that includes Interosseous Membrane between the two bones), and
- the anterior (front) and posterior (back) Tibio-Fibular ligaments.
It generally results from force reverberating through the ankle (e.g., when you slam it into the ground) combined with the rotational stress of turning the foot outward in relation to the leg.
Imagine two basketball players leaping for a rebound and colliding as they hit the ground, with one player’s knee knocking into the other’s. The two lower leg bones may be forced apart, the force causing the ligaments to stretch too far or tear.
It can also happen during side-to-side running, turning while in motion or stopping and starting your feet repetitively.
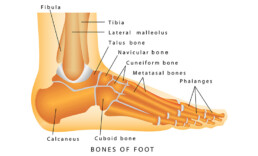
How Do You Know if You Have High Ankle Sprain?
Symptoms of a high ankle sprain may include:
- Minor swelling.
- Significant bruising to the inside, outside and higher portion of the ankle.
- Inability to walk.
- Severe pain.
- Pain when you try to rotate the ankle outward.
- Pain when the ankle is touched.
How Long Does It Take to Recover From a High Ankle Sprain?
When a high ankle sprain occurs, it is with one of three degrees of severity. The recommended treatment for a high ankle sprain depends on the degree of severity involved. They are slower to heal than the more common low ankle sprains. While they heal, your physician may suggest a brace, splint or cast to immobilize the ankle as it heals.
- Grade 1 sprain: This is the mildest variety of sprain with minimal damage to the ligaments, usually accompanied by pain and swelling. These milder sprains are generally treated with rest, ice, elevation and compression. Healing usually takes about six weeks, although you may not be ready to return to action immediately. You may experience joint stiffness and muscle weakness or tightness.
- Grade 2 sprain: These sprains involve extreme stretching of the ligament and may include a partial tear. There is usually significant bruising and swelling under the skin and the ankle is unstable. It generally takes 6 to 12 weeks for recovery.
- Grade 3 sprain: The most severe sprain involves a complete rupture of the ligament and walking is usually difficult. It may require surgery, especially if there is a lot of instability: your surgeon can insert a “syndesmotic screw” between the tibia and fibula to hold the bones in place while the ligament heals and is able to hold the bones in their proper positions. High ankle sprain rehab following surgery generally takes 3 to 6 months.

High Ankle Sprain Rehab
Proper recovery from a high ankle sprain includes three phases, no matter how severe the injury:
- Rest, swelling reduction and protecting the ankle.
- Restoring range of motion, flexibility and strength.
- Returning to normal activities.
Your physiotherapist will be instrumental in the recovery process, providing you with exercises and treatment that will assist you in returning to regular activities. Your physician may also suggest that you wear an ankle brace when you participate in sports.
Prevention
Unfortunately, once you experience a Grade 3 sprain, you are more prone to high ankle sprains. You can attempt to prevent further sprains by:
- Stretching properly before you exercise.
- Warming up beforehand and cooling down afterward.
- Discussing any planned new physical activities with your physiotherapist.
- When participating in high-impact sports, be conscious of your footwork.
- Stay hydrated, especially during the activity.
A high ankle sprain may put you out of action for a while, but with patience and effort, you’ll soon be back in the game.
Suffering From a High Ankle Sprain?
What is a Rotator Cuff Injury?
As the Major League Baseball season heads toward the World Series, its dramatic conclusion, commentators can be heard chattering about the pitchers whose arms are giving them trouble after a long campaign. Often, the words rotator cuff injury are bandied about, drawing moans and groans from the fans. To them, it raises the fear of potential surgery and the possibility that their favourite player won’t be healthy for the following season.
Should you be concerned when you hear those three words, rotator cuff injury? Let’s define the rotator cuff, discuss exactly what a rotator cuff injury is and consider how it can be treated.
The Rotator Cuff Explained
The rotator cuff comprises a group of four small muscles that stabilize and control your shoulder movement. The shoulder is a ball and socket joint, and the muscles come together to form a covering for the ball at the top of the arm bone (humerus) where it fits into your shoulder blade, or scapula.
The rotator cuff is connected to the bone with tendons. To allow the arm bone to glide easily, a lubricating sac called a bursa, separates the rotator cuff from your acromion, the bone at the top of your shoulder.
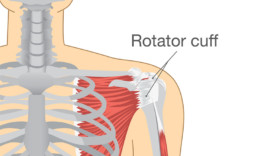
What Is the Best Treatment for Rotator Cuff Injury?
Impingement injuries resulting from overuse respond well to rest and anti-inflammatory medications. Your physiotherapist may also prescribe exercises to help you heal, restore range of motion and strengthen the muscles. Basic exercises for rotator cuff injury that are often used include:
- doorway stretch;
- side-lying external rotation;
- high-to-low rows;
- reverse fly; and
- lawn mower pull.
Rotator cuff tears can be either partial or full. Partial tears result when a part of the rotator cuff pulls away from its attachment to the bone. They rarely require surgery and respond well to rest, ice, physiotherapy, medication and, perhaps, an occasional cortisone injection.
If the tear isn’t healing despite these treatments, there is now the option of having a bioinductive patch applied to the area using minimally invasive arthroscopic surgery. The patch induces the rotator cuff to regenerate and heal itself.
A full tear means the rotator cuff and its tendon are pulled completely away from the bone. If non-surgical means don’t work in treating your injury, or if your job depends on using your rotator cuff, your physician may suggest surgery to repair it. Generally, a surgeon will reattach the tendon to the humerus bone.
The most common surgical options are open repair, which requires a surgical incision; arthroscopy, which requires a tiny incision and uses a microscopic camera to guide the surgeon; and mini-open repair, which combines the two techniques.
Common Rotator Cuff Injuries
Your rotator cuff is protected from minor bumps and knocks by the bones and the ligaments that create an arch over your shoulder. However, injuries can happen, both acute and degenerative.

Acute rotator cuff injuries result from a single incident, such as falling down onto an outstretched arm or using a jerking motion to lift something too heavy.
Degenerative rotator cuff injuries result from wear over time; they can occur naturally as we age. The blood supply to our rotator cuff muscles and tendons lessens, impairing the body’s ability to repair itself.
Rotator cuff injuries can result from the strain of repetitive motion, making tennis players and baseball pitchers susceptible, as well as painters, carpenters and anyone else who does work overhead.
Common rotator cuff injuries include impingements and tears:
- Impingements result when rotator cuff muscles become irritated, swell and obstruct the space between the arm and shoulder bones, causing pinching and irritation to the tendons and bursa.
- Tears and rips – either partial or full – in the rotator cuff muscles or tendons that attach the muscles to the bones.
What Are the Symptoms of Rotator Cuff Tear?
The symptoms for different types of rotator cuff injuries are varied, but common indicators include:
- an arc of shoulder pain or clicking when you lift your arm to shoulder height or overhead;
- shoulder pain that can extend from the top of your shoulder to your elbow;
- shoulder pain when your arm is at rest (usually seen in more severe rotator cuff injuries);
- shoulder pain when you are lying on your sore shoulder;
- shoulder muscle weakness when attempting to reach or lift something;
- shoulder pain when reaching for a seatbelt; or
- shoulder pain when putting your hand behind your back or head.
A rotator cuff injury is best diagnosed using a diagnostic ultrasound scan. Although MRIs are often used to assess the injury, they have been known to miss rotator cuff problems.
If you are experiencing shoulder pain, don’t hesitate to talk to your physician or your physiotherapist. The sooner a rotator cuff injury is diagnosed and treated, the more likely that you’ll have a complete recovery.
Get Relief for Your Rotator Cuff Pain
What is Shoulder Bursitis?
You’ve caught that high fly ball winging its way toward left field with a leap and a grab. As you throw it to third base for the out, you feel pain in your shoulder. Oh, no! Is this the beginning of the end of your career as an amateur outfielder? Will you have to give up a game you so enjoy?
Let’s hope not. What you may be experiencing is bursitis of the shoulder, also known as subacromial bursitis, because it occurs in the bursa beneath your acromion, the bone that forms the roof of your shoulder joint. Very well, you say, but whatever is a bursa?
What Causes Bursitis of the Shoulder?
A bursa (plural, bursae) is a fluid-filled sac that helps to reduce the friction between the bones in a joint and the soft tissues, such as tendons. The bursae lubricate and cushion the areas where these structures rub against each other. Inflammation to these sacs is called bursitis and it may occur in the shoulder, knees, elbows or wrists. Bursitis, while painful, isn’t life-threatening and usually responds well to treatment.
Common causes for shoulder bursitis are:
- Overuse and repetitive movement.
- Sudden injury, such as a blow to the area.
- Aging; formation of calcium deposits on collarbone that interfere with bursa.
- Sudden trauma, e.g., falling so that the shoulder absorbs the blow.
- Lifting items overhead.
- Underlying weakness of the rotator cuff or shoulder blade stabilizers that impinges upon the bursa.
Athletes who use an overhand throwing motion are susceptible to shoulder bursitis, such as swimmers, tennis players and volleyball players. Non-athletes who may experience shoulder bursitis include people involved in chores such as hanging the laundry or painting the house. Shoulder bursitis often occurs as the result of another injury, such as a torn rotator cuff, that begins to impact the bursa.
What Does Bursitis in the Shoulder Feel Like?

The main indicators of the onset of shoulder bursitis are pain and restricted movement:
- Tenderness or stiffness in the affected area.
- Gradual onset of pain that progressively worsens in intensity following or during repetitive activity.
- Rapid onset of pain if caused by trauma.
- Skin may swell and be warm to the touch.
- Pain located at the outside of the shoulder and it may radiate to the mid-arm; it can spread as far as the wrist.
- At rest, shoulder feels more comfortable when held across the body, as if in a sling.
- Pain increases when you lie on the injured side, but it can also hurt when lying on your unaffected side with your arm slung across the body.
- A tightening sensation in the upper arm.
- Pain intensifies when you use your arm for actions that require you to lift it above shoulder height, such as reaching for an object on a high shelf.
- Inability to lift arm away from body, because pain causes a feeling of weakness.
What Is the Best Treatment for Bursitis in the Shoulder?
If you are experiencing shoulder pain that you think might be bursitis, a visit to your physician is indicated. Once he or she diagnoses it, a course of rest and home treatment will generally be successful, but physiotherapy may also help you by strengthening the muscles around your joints; it will certainly be useful in preventing a recurrence.
To heal properly:
- Rest is best. Avoid engaging in any activity that puts pressure on the shoulder or may cause pain.
- Freeze it. As soon as you feel muscle pain or pain near a joint, apply ice for 10 or 15 minutes, as often as twice an hour, if needed. Continue for 72 hours (three days).
- Dull the pain. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen help reduce inflammation and cut the pain.
- Move it. Gently move the affected joint through its full range of motion daily to avoid stiffness. Work with your physiotherapist to add exercises that strengthen the surrounding muscles.
If the swelling is severe, your physician may decide to remove some of the fluid using a needle. He or she might also suggest a pressure bandage for the affected area.
Can Shoulder Bursitis Be Prevented?
Keep your shoulder healthy by:
- Staying the course. Continue with your treatment and exercise regimen.
- Slow but steady. Slowly re-start the activity that aggravated your shoulder, warming up beforehand and stretching afterward. Do the activity for short periods of time to give your body a chance to adjust.
- Improve technique. If a certain activity has caused bursitis, make sure you are doing it with proper technique to avoid further injury. If equipment is necessary, check it to make sure it is doing its job in protecting you.
- Look for alternatives. If the activity that led to injury is a sport you play for fun, consider looking for an alternative that doesn’t require overhead motion.
Remember: shoulder bursitis may be painful, but it can be healed. Be patient and follow the advice of your healthcare professionals and you should soon be feeling fine.
Our Physiotherapists Can Get You Some Relief!
What is Massage Therapy?
Are your neck and shoulders tense from hunching over a computer for eight hours a day? Are you in pain from a sports injury? Perhaps you’re anxious about a big moment in your life, such as a wedding. It’s time to consider a visit to a massage therapist. But what is massage therapy, and who can benefit from it?
Massage Therapy Definition and Applications
The Registered Massage Therapy Association of BC defines massage therapy as the treatment and prevention of dysfunction, injury, pain and physical disorders of the soft tissues and joints by manual and physical methods to develop, maintain, rehabilitate or augment physical function to relieve pain and promote health.
Massage therapists manipulate the body’s soft tissues – muscles, tendons, connective tissues, joints and ligaments – to achieve results. Using touch, therapists:
- relieve pain,
- help heal injuries,
- improve circulation,
- increase relaxation,
- relieve stress,
- reduce muscular tension,
- improve lymphatic drainage, and
- help improve the general wellness of clients.
Massage therapy’s beneficial effect on the body and its ability to optimize health and well-being derives from its acting on the muscular, nervous and circulatory systems.
Massage therapy can be used to develop, maintain and improve physical function and it can relieve or prevent physical dysfunction and pain and the impact of stress on the body. It can be employed to treat both acute and chronic conditions, and it is also effective as a preventive strategy.
Therapeutic Massage Techniques: Types of Massage Therapy

When it comes to therapeutic massage techniques, there are four common types of massage therapy:
- Swedish massage. A gentle form of massage that uses long strokes, kneading, deep circular movements, vibration and tapping to help relax and energize you.
- Deep massage. A massage technique that uses slower, more-forceful strokes to target the deeper layers of muscle and connective tissue, commonly to help with muscle damage from injuries.
- Sports massage. Similar to Swedish massage, this approach is geared toward people involved in sport activities to help prevent or treat injuries.
- Trigger point massage. An approach that focuses on areas of tight muscle fibers that can form in your muscles after injuries or overuse.
Massage Therapists use these massage techniques and others to provide relief for people with a variety of conditions, including:
- Lower back pain,
- Stress,
- Sports injuries,
- Pregnancy,
- Arthritis,
- Fibromyalgia,
- Osteoporosis; and
- Cancer.
However, massage therapy isn’t appropriate in all cases. Avoid it if you have any of the following conditions:
- Bleeding disorders or take blood-thinning medication,
- Burns or healing wounds,
- Deep vein thrombosis,
- Fractures,
- Severe osteoporosis,
- Severe thrombocytopenia.
Massage Therapy Canada – How to Become a Registered Massage Therapist in Canada
Four Canadian provinces regulate massage therapy, just as they do any other healthcare profession. British Columbia, New Brunswick, Newfoundland and Ontario require massage therapists to obtain certification in order to practise as Registered Massage Therapists (RMTs). Many other provinces have professional associations for their massage therapists, and membership is often a sign of appropriate training. The 2011 National Household Survey indicated that there are about 26,000 massage therapists in Canada.
RMTs undergo a rigorous course of education and training to achieve their professional designation – don’t confuse them with employees of massage parlours! Although massage therapy training varies among provinces, it requires comprehensive studies in health sciences such as anatomy, physiology, pathology, kinesiology, orthopedics and neuroanatomy, as well as an understanding of ethics and clinical practice.
How long does it take to become a Registered Massage Therapist in Canada?
Massage therapy programs are generally offered at colleges and last two or three years. In the provinces where registration is required, students must take a certification exam at the conclusion of the course to earn the designation Registered Massage Therapist.
Other provinces also offer massage therapy courses at the college level, but the graduates are not provincially certified or regulated.
Finding a Registered Massage Therapist in Vancouver, BC
Registered massage therapists may practise in a massage therapy clinic, set up in private practice or work as part of a team of healthcare professionals, including physiotherapists, physicians, nurses and social workers.
If you need to find a registered massage therapist in Vancouver, BC, you can ask your physician or physiotherapist to recommend an RMT, or you can contact a professional association, such as the Registered Massage Therapists of British Columbia, for a recommendation. In provinces where the profession isn’t regulated, there are also professional associations for massage therapists and they have a roster of members to suggest.
Visiting a Massage Therapist
If you haven’t visited a massage therapist in the past, you may be a bit anxious at the thought of someone you don’t know touching you. Relax. Massage therapists are healthcare professionals and they are trained to be sensitive to your concerns. They are also bound by professional ethics to treat you professionally and with appropriate care.
Your first appointment will undoubtedly remind you of a visit to your doctor. The RMT will ask about your medical history, your current health, your reasons for coming and any medications you are taking. They will assess your needs and suggest the therapeutic massage technique that they feel will best address your issues. You always have the right to disagree or refuse specific types of treatment.
Once you’ve enjoyed the health benefits of a therapeutic massage, you’ll be ready to return as often as you can. The relaxation and muscle relief are extremely satisfying and effective.
Looking for Vancouver's top Massage therapist?
How to Treat a Pinched Nerve
As a child growing up, you, like most of us, were probably victimized on occasion by a sibling who pinched you for effect: the resulting screeches tend to be dramatic. A pinched nerve may not cause you to howl with the same pain and indignation, but it is unpleasant and requires tending. Unfortunately, calling for your mother to punish the offender isn’t an acceptable solution in this case!
What Is a Pinched Nerve?
Nerves are the highways and roads extending throughout our body to carry signals to and from the brain. When the surrounding tissues – cartilage, bones, muscles or tendons – place too much pressure on a nerve and pain and/or other symptoms result, it is called a pinched nerve.
You can experience pinched nerves at a variety of places throughout the body. For example, you may have a pinched nerve in your wrist, causing carpal tunnel syndrome, or a herniated disc that results in a pinched nerve somewhere in your spine. Many people experience a pinched nerve in their neck, shoulder, lower back, arm and feet.
What Causes a Pinched Nerve?
Some of us are more prone to pinched nerves than others. Your susceptibility is increased if you exhibit any of the following characteristics:
- Female sex. Women are more likely to develop carpal tunnel syndrome.
- Bone spurs. If trauma or injury causes a bone spur, it can narrow the passage for nerves to travel, leading to a pinched nerve.
- Thyroid disease. If you have thyroid problems, you are more prone to carpal tunnel syndrome.
- Rheumatoid arthritis. Arthritis often causes inflammation, which puts pressure on your joints.
- Diabetes. People with diabetes have a higher risk of pinched nerves.
- Overuse. If you participate in sports or hobbies that require repetitive motion, you stand at risk of a pinched nerve.
- Prolonged bed rest. Lying down for long periods can lead to compression of your nerves.
- Pregnancy. Pregnant women are susceptible to pinched nerves due to the pressure put on nerves by weight gain and water retention.
- Obesity. Carrying excess weight can place pressure on your nerves.
Pinched Nerve Symptoms
If you have a pinched nerve somewhere in your body, you may experience one or more of these sensations:
- Numbness or decreased sensation in the area supplied by the nerve.
- Frequent feeling that a foot or hand has “fallen asleep”.
- Muscle weakness in the affected area.
- Sharp, aching or burning pain, which may radiate outward.
- Tingling, pins and needles sensations (paresthesia).
- Burning or hot and cold sensations.

How Is a Pinched Nerve Diagnosed?
The connection between a pinched nerve and its symptoms may not be obvious, because the pain may not appear at the source; it may be felt further down the path from the affected nerve. Your spine, however, is a very intricate structure, so any changes to the surrounding muscles or tendons may have an impact.
If your physician suspects a pinched nerve, you may be asked to undergo one or more tests to determine whether your nerve is pinched and/or damaged:
- Magnetic resonance imaging (MRI). A magnetic field and radio waves produce images of your body on multiple planes.
- Electromyography (EMG). EMG evaluates the electrical activity of your muscles when they’re active and when they are at rest.
- High-resolution ultrasound. Sound waves produce images of your body’s structures, allowing assessment of damage.
- Nerve conduction study. Electrodes measure electrical nerve impulses and muscle function.
How Do You Relieve a Pinched Nerve?
No matter whether the pain you are experiencing is minor or strong, it’s important to address it quickly so that you don’t sustain permanent nerve damage. Your physician will discuss options of how to treat a pinched nerve with you based on your condition.
In most cases your physician will turn first to non-invasive treatment options:
- Rest. The first remedy your physician may suggest is rest of the affected area to allow healing. This may include wearing a splint to keep it immobile, depending on the location of the nerve.
- Hot and Cold Therapy. Treating the affected area with heating pads and ice packs, used alternately according to instructions, may relieve mild pain.
- Posture. Aligning the spine properly to distribute your body weight across it evenly can relieve pressure.
- Physiotherapy. Physiotherapists can perform spinal traction (decompression), and teach you proper stretching and strengthening exercises to support the spine. They can help you increase the endurance and flexibility of the surrounding muscles, especially in the target area, to relieve pressure on the nerve and ease pain. They can also suggest ways to modify movements that aggravate the affected nerve.
- Massage. A registered massage therapist can use deep therapeutic massage to increase blood flow and promote healing, while relieving pain.
After a few weeks or months, if these non-invasive treatments aren’t bearing fruit, your physician may suggest surgery to relieve the pressure on the nerve. The good news is that, in most cases, you can treat the injury yourself with help from the aforementioned professionals.