How to Deal with a Crick in the Neck: Effective Remedies and Prevention Strategies
A crick in the neck is a common and often bothersome condition that many of us have experienced at one point or another. It usually manifests as a sharp pain or stiffness in the neck that can make it difficult to turn your head or sleep comfortably. While typically not serious, a crick in the neck can significantly impact your daily life, affecting your comfort and mobility. This article will explore what a crick in the neck is, its common causes, and practical ways to relieve discomfort and prevent future occurrences.
Understanding a Crick in the Neck
A crick in the neck is often used to describe a stiff neck or a feeling of discomfort and restricted movement in the cervical spine. This condition can result from a variety of factors, including muscle strain, poor sleeping position, or holding your neck in an awkward position for an extended period. Although most cricks resolve themselves within a few days, understanding how to manage and prevent them can provide relief and minimize recurrence.
Common Causes of a Crick in the Neck
1. Muscle Strain or Sprain
– Overuse or sudden movements can strain the neck muscles, leading to stiffness and pain. This is common after heavy lifting or vigorous exercise without proper warm-up.
2. Poor Posture
– Prolonged periods of poor posture, such as hunching over a desk or slouching while using electronic devices, can contribute to muscle tension and lead to a crick.
3. Awkward Sleeping Positions
– Sleeping in an awkward position, such as with inadequate neck support, can lead to stiffness upon waking. Using too many pillows or an overly soft mattress can exacerbate this issue.
4. Stress and Tension
– Emotional stress often manifests physically, leading to muscle tension and knots in the neck area, which can result in pain and limited mobility.
5. Cold Drafts or Sudden Temperature Changes
– Exposure to cold drafts can cause muscles to contract, leading to stiffness and discomfort in the neck area.
4. Massage Therapy
– Gentle massage of the neck and shoulders can alleviate muscle tension and promote relaxation. Self-massage using the fingertips to apply gentle pressure can also be effective.
5. Physiotherapy
– Consulting a physiotherapist can be highly beneficial for addressing a crick in the neck. A physiotherapist will assess your condition and develop a personalized treatment plan, which may include targeted exercises to strengthen and stretch neck muscles, manual therapy techniques to relieve pain and improve mobility, and ergonomic advice to prevent future issues. Regular physiotherapy sessions can help ensure a quicker recovery and reduce the likelihood of recurrence.
6. Proper Rest and Relaxation
– Ensure adequate rest and avoid strenuous activities that could exacerbate your condition. Practicing relaxation techniques, such as deep breathing or meditation, can also help reduce muscle tension.
7. Maintain Good Posture
– Be mindful of maintaining good posture throughout the day. Ensure your workstation is ergonomically designed, and avoid prolonged periods in awkward positions.
Integrating physiotherapy into your treatment plan can be an effective way to manage and resolve a crick in the neck. With the right combination of home remedies and professional care, you can alleviate discomfort and promote long-term neck health. If your neck pain persists or worsens, seeking advice from a healthcare professional or physiotherapist is crucial for comprehensive evaluation and treatment.
Prevention Strategies for a Crick in the Neck
1. Ergonomic Adjustments
– Set up your desk or workspace to maintain a neutral neck position, with monitors at eye level. Use an ergonomic chair with adequate support.
2. Regular Stretching and Exercise
– Incorporate regular stretching and strengthening exercises for your neck and upper back muscles into your routine. Activities like yoga and Pilates can promote flexibility and posture.
3. Mindful Movements
– Be cautious with quick movements that can strain the neck. Pay attention to how you move, especially when lifting heavy objects or exercising.
4. Choose the Right Pillow and Mattress
– Use a supportive pillow that maintains your neck’s natural curve while sleeping. A mattress that’s neither too hard nor too soft can help maintain good spinal alignment.
5. Manage Stress
– Implement stress-reducing activities like mindfulness, meditation, or gentle exercise to prevent muscle tension and cricks in the neck.
A crick in the neck can be uncomfortable, but with the right approaches, you can alleviate pain and prevent future incidents. By understanding the causes and integrating effective remedies and prevention strategies, you can maintain neck health and enjoy greater flexibility and comfort in your daily activities. If your neck pain persists or worsens, consider consulting with a healthcare professional or physiotherapist for further evaluation and treatment.
Effective Remedies for a Crick in the Neck
1. Apply Heat or Cold
– Applying a heating pad or warm compress helps relax tight muscles and improve blood flow. Alternatively, an ice pack can reduce inflammation and numb sharp pain. Use each method for 15-20 minutes every hour as needed.
2. Gentle Stretching and Movement
– Perform slow, gentle stretches to relieve tension. Easy neck rolls, side bends, and chin tucks can help increase mobility and reduce stiffness.
3. Over-the-Counter Pain Relief
– Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help manage pain and inflammation. Always follow dosing instructions and consult with a healthcare professional if needed.
Prevention Strategies for Deep Knots in Shoulder Blades
Preventing deep knots in the shoulder blades involves a proactive approach to health and wellness. Incorporate the following strategies into your lifestyle:
– Maintain good posture at work, especially during extended periods of sitting.
– Take frequent breaks to stretch and move around, promoting healthy blood flow.
– Warm up adequately before engaging in physical activities to avoid muscle strain.
– Practice stress reduction techniques to limit muscle tension.
– Pay attention to early signs of muscle discomfort and address them promptly to prevent worsening.
Deep knots in the shoulder blades can be painful and disruptive, but a combination of effective treatments and preventive strategies can help alleviate symptoms and restore mobility. If you experience persistent or severe pain, consult with a healthcare professional or physiotherapist for personalized evaluation and treatment, ensuring you regain optimal shoulder health and function.
Deep Knots in Shoulder Blades: Symptoms, Causes, and Treatment
Shoulder discomfort is a common issue that can arise from various causes, and one prevalent complaint is the presence of deep knots in the shoulder blades. These knots, often referred to as muscle knots or trigger points, can cause significant pain and stiffness, impacting daily activities and overall quality of life. This comprehensive guide explores the symptoms, underlying causes, and effective treatments for deep knots in the shoulder blades, helping you understand how to alleviate this discomfort and prevent future occurrences.
What Are Muscle Knots?
Muscle knots are areas of tense and contracted muscle fibers that have tightened and formed painful nodules. They can occur in various parts of the body but are particularly common in the shoulder region. Known scientifically as myofascial trigger points, these knots can result from muscle overuse, stress, or poor posture, leading to inflammation and discomfort.
Symptoms of Deep Knots in the Shoulder Blades
Identifying the symptoms of deep muscle knots is the first step in addressing the problem effectively. Common symptoms include:
1. Localized Pain and Tenderness
– A deep ache or sharp pain in the shoulder blades or upper back area.
– The affected area is often tender to the touch, with increased sensitivity.
2. Muscle Stiffness and Limited Range of Motion
– Difficulty moving the shoulders or neck freely due to tight and restricted muscles.
– Reduced ability to perform daily activities that involve shoulder or arm movement.
3. Referred Pain
– Pain radiating to nearby areas, such as the neck, arms, or lower back, due to interconnected muscle fibers.
– Headaches or tension-type pain can result from muscle knots around the shoulder blades.
4. Muscle Tightness or Spasms
– A feeling of tightness or persistent muscle tension in the upper back region.
– Occasional muscle spasms may occur due to increased strain on surrounding muscle groups.
5. Fatigue
– Due to constant pain or discomfort, individuals may experience fatigue or a reduced ability to concentrate.
Causes of Deep Knots in the Shoulder Blades
Muscle knots can develop for various reasons, including:
1. Poor Posture
– Slouching or hunching over computers and mobile devices leads to imbalances in muscle alignment and strain in the shoulder and upper back region.
2. Muscle Overuse
– Repetitive activities or prolonged use of specific muscle groups can cause overuse injuries, resulting in knots forming due to muscle exhaustion.
3. Stress and Tension
– Emotional stress can manifest physically, leading to muscle tension and the development of knots in the shoulder area.
4. Inadequate Warm-Up or Stretching
– Engaging in physical activities without proper warm-up or stretching can strain muscles and contribute to the formation of knots.
5. Injury or Trauma
– Direct injuries or accidents affecting the shoulder area can lead to muscle knots as the body attempts to protect the affected area.
Effective Treatment for Deep Knots in the Shoulder Blades
Addressing muscle knots involves a combination of treatments aimed at relieving pain and restoring muscle function. Consider the following approaches:
1. Physical Therapy
– A physiotherapist can assess your condition and provide targeted treatments to address muscular knots, including manual therapy, stretching, and strengthening exercises.
2. Massage Therapy
– Regular massage therapy helps reduce muscle tension and enhance blood circulation, promoting relaxation and knot release.
3. Trigger Point Therapy
– Specialized trigger point therapy, focusing on releasing tension in specific areas, can effectively alleviate muscle knots.
4. Heat and Cold Therapy
– Using a heating pad or warm compress eases muscle tightness, while cold therapy reduces inflammation.
5. Stretching and Mobility Exercises
– Incorporating daily stretching routines and mobility exercises for the shoulders and upper back helps maintain flexibility and reduce stress on muscles.
6. Posture Correction
– Pay attention to your posture by setting up an ergonomic workspace and consciously maintaining proper alignment throughout the day.
7. Stress Management
– Practice relaxation techniques such as deep breathing, yoga, or meditation to manage stress and reduce muscle tension.
8. Hydration and Nutrition
– Staying hydrated and maintaining a balanced diet supports muscle health and reduces the likelihood of developing knots.
Prevention Strategies for Deep Knots in Shoulder Blades
Preventing deep knots in the shoulder blades involves a proactive approach to health and wellness. Incorporate the following strategies into your lifestyle:
– Maintain good posture at work, especially during extended periods of sitting.
– Take frequent breaks to stretch and move around, promoting healthy blood flow.
– Warm up adequately before engaging in physical activities to avoid muscle strain.
– Practice stress reduction techniques to limit muscle tension.
– Pay attention to early signs of muscle discomfort and address them promptly to prevent worsening.
Deep knots in the shoulder blades can be painful and disruptive, but a combination of effective treatments and preventive strategies can help alleviate symptoms and restore mobility. If you experience persistent or severe pain, consult with a healthcare professional or physiotherapist for personalized evaluation and treatment, ensuring you regain optimal shoulder health and function.
Turtle Neck Syndrome: Causes, Symptoms, and Solutions
What is Turtle Neck Syndrome?
In today’s digital age, it’s common to find ourselves glued to our screens for prolonged periods, whether it’s for work, study, or leisure. This lifestyle change has given rise to a musculoskeletal condition known as “Turtle Neck Syndrome,” also referred to as “Tech Neck” or “Text Neck.” This syndrome is becoming increasingly prevalent as our reliance on electronic devices grows. This comprehensive guide will explore Turtle Neck Syndrome, its causes, symptoms, and effective remedies to alleviate discomfort and prevent future issues.
Turtle Neck Syndrome is a modern ailment defined by repetitive stress injury and pain in the neck area, primarily caused by the repetitive strain of holding the head in a forward and downward position. This posture is most commonly associated with the use of smartphones, tablets, laptops, and even desktop computers over extended periods. The term “turtle neck” derives from the resemblance of one’s posture to that of a turtle poking its head out of its shell, with the neck craned forward.
Causes of Turtle Neck Syndrome
The primary cause of Turtle Neck Syndrome is poor posture due to prolonged use of digital devices. Here are some common factors that contribute to the development of this syndrome:
1. Prolonged Device Use
In today’s digital era, our dependency on smartphones and tablets has skyrocketed. Whether it’s for communication, entertainment, or work, we often find ourselves glued to these devices for hours on end. When using these devices, our natural inclination is to hold them below eye level, which forces us to tilt our heads downward. This consistent downward gaze increases the gravitational force on the neck muscles, leading to strain. The human head weighs approximately 10-12 pounds, but the force exerted on the neck increases dramatically the further forward the head tilts. Over time, this repeated strain can lead to muscle fatigue, pain, and inflammation, setting the stage for Turtle Neck Syndrome.
2. Poor Ergonomics
A growing number of individuals are working from home or in flexible workspaces, often without proper ergonomic setups. Desks at inappropriate heights, chairs lacking sufficient support, low computer monitors, and poorly positioned keyboards can all contribute to poor posture. When the workstation is not ergonomically designed, individuals tend to adjust their bodies to meet the environment, typically by hunching over or craning their necks forward. This poor alignment leads to sustained abnormal neck positioning, placing undue stress on the cervical spine and surrounding muscles. Over time, such poor workplace ergonomics can significantly contribute to the development of Turtle Neck Syndrome.
3. Lack of Physical Activity
The modern lifestyle has become increasingly sedentary, with many individuals spending a large portion of their day sitting at a desk or in front of a computer. Physical inactivity can weaken the muscles that support the neck and upper back, making it difficult to maintain good posture. When these muscles are underdeveloped, they cannot adequately support the head’s weight, leading to forward head posture and increased strain on the cervical spine. Lack of regular exercise also contributes to reduced flexibility and joint stiffness, exacerbating the development of postural issues like Turtle Neck Syndrome.
4. Inadequate Breaks
In a fast-paced work environment, taking breaks might seem counterproductive, but neglecting to do so can have serious consequences for neck health. Continuous work, particularly if it involves staring at a screen, can lead to repetitive stress on the neck muscles without any relief. Skipping breaks means missing out on the opportunity to stretch, move, and reset one’s posture, which is vital to counteracting the effects of extended periods of sitting or device use. Regular breaks allow the muscles to relax and recover, reducing the cumulative stress and strain that contribute to Turtle Neck Syndrome. Without them, tension builds up, leading to chronic pain and discomfort.
5. Repetitive Movements
Modern digital habits like texting or typing encourage repetitive neck movements, such as frequent nodding or looking down at a device. These movements, when performed consistently over time, can overwork the neck muscles and lead to imbalances. For example, typing on a laptop or holding a smartphone involves repetitive actions that put undue pressure on the cervical spine by maintaining a bent-forward posture. Each of these repeated actions might seem harmless on its own, but collectively, they contribute to muscle tightness, joint wear and tear, and nerve irritation. This repetitive stress is a significant factor in developing Turtle Neck Syndrome and can also worsen existing neck conditions.
By understanding and addressing these factors, individuals can take proactive steps to reduce their risk of developing Turtle Neck Syndrome. This can include adjusting their workspace for better ergonomics, incorporating more physical activity into their daily routine, taking regular breaks to stretch and move, and being mindful of their posture while using digital devices.
Symptoms of Turtle Neck Syndrome
The symptoms of Turtle Neck Syndrome can vary in severity from one individual to another, with common indicators including:
– Neck Pain and Stiffness: A throbbing or sharp pain in the neck, often worsening with activity.
– Reduced Mobility: Difficulty in moving the head freely, resulting in a loss of range of motion.
– Headaches: Tension headaches originating from the scalp, neck, and upper back muscles.
– Shoulder Tension and Pain: Muscle tension extending to the shoulders and sometimes the upper back.
– Postural Changes: The head tilts forward beyond its normal alignment, leading to a noticeable “hump” or rounding of the upper back.
– Nerve Pain: Tingling or numbness in the arms and hands caused by nerve compression in the cervical region.
Fixes and Prevention Strategies for Turtle Neck Syndrome
While Turtle Neck Syndrome can be inconvenient and painful, various strategies can help manage and prevent the condition. Ergonomic adjustments are crucial for reducing the risk of developing Turtle Neck Syndrome and promoting overall musculoskeletal health. By optimizing your work environment, you can alleviate unnecessary strain on your neck and spine, leading to improved comfort and productivity. Let’s explore how specific ergonomic changes can make a significant impact:
1. Optimal Screen Height
Ensuring your screen is at eye level is one of the most effective adjustments you can make to prevent neck strain. When your computer screen is too low, it forces you to tilt your head forward, increasing the load on your neck and upper back muscles. This posture, if maintained for extended periods, leads to muscle fatigue and can ultimately cause chronic neck pain. By positioning your screen at eye level, you maintain a neutral neck position, minimizing the forward head posture and distributing the weight of your head more evenly along your spine. Use monitor stands, adjustable desks, or stack books under your laptop to achieve the optimal screen height, allowing one to maintain a comfortable viewing angle without straining the neck.
2. Chair Support
Investing in a good ergonomic chair with adequate lumbar support is essential for maintaining a healthy sitting posture. The lumbar region of the spine naturally curves inward, and a chair with proper lumbar support helps maintain this natural curvature. When sitting, ensure your back is fully supported by the chair, and your feet are flat on the ground, with knees at a right angle. The right chair will promote an upright sitting posture, reducing the tendency to slouch or lean forward. Features such as adjustable seat height, depth, and tilt further allow the chair to fit your body dimensions, ensuring comfort during prolonged periods of sitting. By properly supporting your lower back, you reduce the strain on your neck and shoulders, helping to prevent Turtle Neck Syndrome.
3. Keyboard and Mouse Position
The correct positioning of your keyboard and mouse is vital in preventing repetitive strain injuries and promoting a healthy posture. When your keyboard and mouse are at the wrong height or distance, they can cause you to hunch your shoulders or extend your arms awkwardly, leading to neck and shoulder tension. To prevent this, position your keyboard so that your elbows remain at a 90-degree angle when typing, with your wrists straight and your upper arms relaxed at your sides. Your mouse should be easily accessible without needing to stretch or twist your wrist. Consider using a keyboard tray, ergonomic keyboard, or mouse pad with wrist support to maintain a neutral wrist position. Keeping everything within comfortable reach not only prevents hunching but also encourages a relaxed shoulder posture, decreasing the likelihood of developing musculoskeletal issues.
Incorporating these ergonomic adjustments can make a significant difference in reducing neck and back strain, enhancing comfort, and preventing the onset of Turtle Neck Syndrome. By taking the time to assess and optimize your workspace, you contribute to maintaining a healthier posture, boosting your physical well-being and productivity.
Physical Exercises and Stretches for Turtle Neck Syndrome
1. Chin Tucks: Gently tuck your chin towards your chest and hold for a few seconds, repeatedly. This exercise strengthens neck muscles.
2. Neck Rolls: Slowly roll your neck in a clockwise and then counterclockwise direction to enhance flexibility.
3. Shoulder Blade Squeezes: Draw your shoulder blades back and together, holding the position briefly to strengthen the upper back.
4. Wall Angels: Stand with your back against the wall, slide your arms up and down the wall like a snow angel to improve posture and shoulder mobility.
Lifestyle Modifications: Turtle Neck Syndrome
Lifestyle modifications play a crucial role in preventing Turtle Neck Syndrome, especially in today’s tech-centric world. By integrating simple yet effective changes into your daily routine, you can reduce the risk of neck and back strain, promote better posture, and enhance overall well-being. Let’s explore these modifications in detail:
1. Frequent Breaks
Taking regular breaks from screen time is essential for alleviating muscle tension and preventing the repetitive stress that contributes to Turtle Neck Syndrome. Every 30 minutes, step away from your screen to stretch and move around. These breaks don’t have to be long—just a few minutes of walking or stretching your neck, back, and shoulders can suffice. Use this time to perform quick exercises such as shoulder rolls, gentle neck stretches, or standing up to relax tight muscles and reset your posture. Implementing techniques like the Pomodoro Technique, which includes taking short breaks after focused work intervals, can help ensure you incorporate these reprieves consistently throughout your day.
2. Conscious Posture Awareness
Developing a habit of conscious posture awareness can significantly impact your neck and spine health. Regularly check your posture throughout the day, especially during prolonged periods of sitting or screen use. Ensure your back is straight, shoulders are relaxed, and your head is aligned over your spine. Set reminders on your phone or computer to cue these posture checks. With time, these visual or audio reminders will become internalized, helping you automatically correct your posture without having to think about it. Being aware of how you carry yourself and making adjustments as needed can prevent the development of poor posture habits that contribute to musculoskeletal discomfort.
3. Limit Screen Time
Reducing non-essential screen time is an effective way to minimize the risk of Turtle Neck Syndrome. Evaluate your daily routine to identify unnecessary electronics use, such as excessive social media scrolling or binge-watching. Set boundaries or time limits for using digital devices, and replace these activities with offline hobbies or social interactions. Engaging in activities that do not require screen use, like reading a physical book, exploring outdoors, or pursuing creative pastimes, can provide a refreshing break for your eyes and neck. By decreasing overall screen exposure, you reduce the frequency and duration of looking down or straining your neck, promoting better posture and overall health.
4. Physical Activity
Incorporating regular physical activity into your daily routine is crucial for strengthening the muscles that support your neck, shoulders, and back. Exercise enhances muscle tone and flexibility, which are essential for maintaining good posture. Engage in exercises that target these muscle groups, such as resistance training with weights, yoga, or Pilates. Specific exercises like shoulder shrugs, neck rotations, and back extensions can be particularly beneficial. Regular aerobic activity, such as walking, cycling, or swimming, can also improve cardiovascular health and help prevent weight gain, which can adversely affect posture. A well-rounded fitness regimen supports musculoskeletal health and helps you sustain an upright posture throughout daily activities.
By implementing these lifestyle modifications, you take proactive steps to prevent Turtle Neck Syndrome and enhance your physical well-being. These changes not only mitigate the strain associated with prolonged device use but also foster a healthier, more balanced lifestyle.
Professional Interventions for Turtle Neck Syndrome
1. Physiotherapy: Consult a physiotherapist for a personalized exercise program designed to address your symptoms.
2. Massage Therapy: Regular massages can relieve muscle tension and improve circulation in the neck and upper back.
Turtle Neck Syndrome is a common ailment in today’s tech-driven world, but with awareness and proactive practices, it is manageable. Through ergonomic changes, regular exercises, and potential professional assistance, you can alleviate symptoms and maintain a healthy posture. Remember, small changes in your daily habit can lead to significant improvements in your overall well-being. Stay conscious of your posture and make regular efforts to stand tall—your neck will thank you for it!
Best Knee Wrap for Baker's Cyst: a Guide
What is a Baker’s cyst?
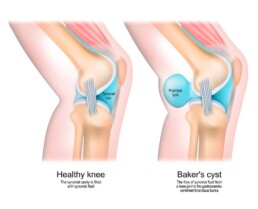
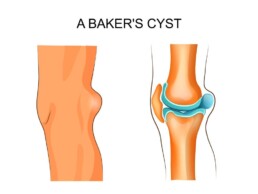
A Baker’s cyst is a fluid-filled sac that develops on the back of the knee due to an excess of the synovial fluid that lubricates the interior of the knee. This type of cyst is named after William Morrant Baker, the 19th-century physician who was the first to describe the condition. It is also called a popliteal cyst, referring to the area behind the knee.
Synovial fluid not only lubricates all the body’s joints; it reduces friction there. A tear in the knee’s cartilage or inflammation from arthritis can result in an overproduction of the fluid. The build-up of this excess fluid becomes a Baker’s cyst. It may also be caused by poor leg biomechanics.
A small Baker’s cyst may not produce symptoms, but a larger cyst may be accompanied by pain and swelling and can restrict the degree to which the knee can bend. The symptoms vary, but they can include:
- Stiffness or tightness in the back of the knee, thigh, or upper calf.
- Pain behind the knee, particularly with full flexion (bending) or extension (straightening). You may also experience pain in the upper calf or back of the thigh.
- Pain when sitting when the chair touches or rubs the area behind the knee.
- Swelling and redness behind the knee. If the cyst ruptures, then the swelling may be also be in the lower leg and calf area. It usually worsens when standing.
- Fatigue and restless leg at night.
Diagnosis
A Baker’s cyst may be located below the skin, so it may not be visible to the eye. In diagnosing it, your physician should employ range of motion testing, palpation and observation of swelling patterns. They should also ask you about your medical history to determine whether you have had any recent knee trauma or suffer from any arthritic conditions. An MRI or ultrasound may be required, especially because the symptoms are similar to those of other knee problems.
Often, a Baker’s cyst will resolve on its own over time, given rest and treatment of symptoms. However, your physician may prescribe a course of anti-inflammatory medication (orally), a cortisone injection, aspiration of the fluid by utilizing a needle, and/or surgical removal.
Physiotherapy can assist you in regaining your mobility and maintaining your fitness so that the cyst doesn’t recur. A registered physiotherapist may use acupuncture or dry needling to aid your healing and will work with you to restore your range of motion and strengthen the quadriceps and hip abductor muscles, areas where weakness often contributes to poor biomechanics.
Treatment: Is It Good to Wrap a Baker’s Cyst?
Initially, if you suspect a Baker’s cyst, you can follow the RICE protocol: rest, ice, compression and elevation. Remember, rest may prompt the cyst to heal on its own. When you ice the cyst, never put the ice directly onto bare skin; wrap it in a towel for protection or use a bag of frozen peas. Ice your cyst for no more than 20 minutes each hour.
You may want to wrap the knee, since compression is known to decrease swelling. Before you consult with your doctor or physiotherapist, you can use an ACE bandage or a pair of thigh-high (NOT knee-high) compression socks.
What Makes the Best Knee Wrap for Baker’s Cyst?
Once you are certain you have a Baker’s cyst, ongoing compression may help you heal. The best knee wrap for your cyst combines compression, ice and stability. Compression is an excellent method of lessening the swelling and allowing the fluid to reabsorb. Ice is a great way to reduce the pain caused by the cyst and can prevent the need for medication. Stability is important if the cyst was caused by damage to the joint or degenerative changes.
Here are three types of knee wraps that are worth considering:
- Knee Compression Sleeve. An elastic bandage is easy to slide on and off and is comfortable for you to wear. It helps reduce swelling.
- Knee Brace with Ice Pack Wrap. A compression knee brace with Velcro closures that also has space to insert ice that cools the back of the knee – two keys to relieving pain and reducing swelling.
- Decompression Knee Brace. If your knee is unstable, especially if there have been degenerative changes to the joint, consider a hinged brace that provides both compression and lateral stability.
Remember: while you are suffering from a Baker’s cyst, listen to your physiotherapist’s advice regarding exercise, and IF IT HURTS, DON’T DO IT!
Pulled Glute Muscle: How to Treat a Pulled Gluteus Maximus
Your gluteus maximus is a powerful muscle that helps you perform many everyday activities. It’s easy to take this muscle for granted until it starts to hurt, feels tighter than usual, or you’re unable to move as freely. When these issues arise, it’s natural to worry that you might have pulled a muscle or need medical treatment.
Knowing how to recognize and treat a pulled gluteus maximus can help you stay active and healthy. However, it’s important to understand that muscle injuries often need professional medical attention. Let’s dive into what the gluteus maximus is and how you can take care of it.
What is the Gluteus Maximus?
The gluteus maximus is the large muscle in your lower back and buttocks. It’s part of a trio known as the gluteal muscles, which also includes the gluteus medius and the gluteus minimus. The gluteus maximus is not only the largest muscle in your buttocks but also the strongest of the three.
Why is the Gluteus Maximus Important?
This muscle plays a vital role in:
- Maintaining Balance and Stability: It helps protect your spine and keeps you steady.
- Hip Movements: It's responsible for extending your hip (like when you stand up), moving your leg away from your body (abduction), and rotating your hip outward.
- Daily Activities: Whether you're standing, walking, running, or jumping, the gluteus maximus is hard at work.
- Stabilizing the Hip Joint: It provides crucial support to your hip during movement.
Why Does it Hurt?
When the gluteus maximus is tight or injured, you might experience pain, reduced range of motion, and less stability. This can impact your ability to carry out everyday tasks.
Recognizing a Pulled Gluteus Maximus
If you suspect you’ve pulled your gluteus maximus, look out for:
- Pain and Soreness: This can appear in your lower back, buttocks, or hip area.
- Tightness: The muscle may feel stiffer than usual.
- Limited Movement: You might find it hard to move as freely as before.
- Weakness: The affected area might feel weaker or less stable.
What Can You Do When You Pulled a Glute Muscle?
While it’s best to seek medical advice for any significant discomfort, here are some general tips for caring for your gluteus maximus:
- Rest: Give the muscle time to heal by avoiding activities that cause pain.
- Ice and Heat: Applying ice can reduce swelling, while heat can help relax tight muscles.
- Gentle Stretching: Once the initial pain subsides, gentle stretching can help improve flexibility.
- Strengthening Exercise: Building strength in the gluteus maximus, gluteus medius, and gluteus minimus can enhance stability and prevent future injuries.
Prevention is Key to Preventing a Pulled Glute Muscle?
Regular stretching and strengthening of the gluteus maximus can help keep this muscle healthy and prevent injuries. Incorporating these practices into your routine can make a significant difference in your overall well-being.
If you have concerns about your gluteus maximus or experience persistent pain, don’t hesitate to consult a healthcare professional. Taking prompt action can help you get back on your feet and stay active.
Gluteus Maximus Injuries: What You Need to Know
Given how much work your gluteus maximus muscles do, it’s no wonder they’re susceptible to injury. Here are some common types of gluteus maximus injuries and what you should know about them:
1. Sprains
Sprains happen when the ligaments that connect your gluteus maximus to your bones get stretched or torn. This can occur due to sudden movements, like a quick twist, or from repetitive activities like walking or running on uneven surfaces.
2. Pulls/Strains
Pulls or strains occur when the muscle is stretched beyond its usual limits, causing tiny tears or microtears in the muscle fibers. This leads to pain, swelling, and a restricted range of motion.
3. Tears
Tears are more severe and happen when a strong force causes a complete rupture of the muscle fibers. This can result in significant pain and functional limitations.
Why Do These Injuries Happen?
Anyone can experience these injuries, but they are more common in people who don’t take the time to warm up and cool down properly before and after exercise or intense activities.
Symptoms of a Gluteus Maximus Injury
If you think you might have injured your gluteus maximus, look out for these symptoms:
- Pain in the Buttocks: This can range from mild discomfort to sharp, intense pain.
- Stiffness in the Buttocks/Hips: Making it hard to move freely.
- Visible Swelling: You might notice a bulge or swollen area.
- Tenderness: The area may be sensitive to touch.
- Discomfort When Sitting/Standing/Bending: Everyday activities might become painful.
The severity of your symptoms can vary depending on the type and extent of the injury, ranging from very mild to severe.
At-Home Treatments for Minor Strains
For minor strains, here are some simple steps you can take to feel better:
Rest and Ice: Take a few days off from exercise and apply ice to the affected area to reduce swelling and pain.
Light Stretching: Gentle stretches can help maintain flexibility and reduce tightness. Here are a few you can try:
1. Bridge Stretch:
– Lie on your back with your knees bent and feet flat on the floor.
– Slowly lift your hips until you feel a stretch in your buttocks.
– Hold for a few seconds, then lower your hips back down.
– Repeat as needed.
2. Hamstring Stretch:
– Lie flat on your back.
– Lift the affected leg until you feel a stretch in the back of your leg.
– Hold for 10 seconds and then switch to the other leg.
3. Seated Hip Rotator Stretch:
– Sit in a chair and cross one leg over the opposite knee (so your foot rests on the knee).
– Lean forward gently until you feel a slight stretch in your hip.
– Hold for 10-15 seconds, then release and switch to the other leg.
Physiotherapy Treatment for a Gluteal Strain
Once you’ve gotten past the initial rest and icing phase, it’s important to start rehabilitating your gluteal muscle. Physiotherapy can play a key role in your recovery.
Your physiotherapist may also use specific treatments to support your rehabilitation, such as:
Electrotherapy: Uses electrical signals to help reduce pain and speed up muscle healing.
Massage: Helps relieve muscle tightness and improve blood flow.
Stretching Exercises: Keeps the muscle flexible and prevents stiffness.
Mobilization Exercises: Enhances your overall range of motion.
Education on Activity and Technique: Your physiotherapist will teach you how to move properly to avoid re-injury and improve your overall technique.
Remember, the goal is to get you back to doing the things you love without pain or discomfort. With physiotherapy and a guided rehabilitation program, you’ll be well on your way to recovery!
Do you think you may have pulled your Glute?
Hypertonic Pelvic Floor
A hypertonic pelvic floor refers to the condition where the muscles in the pelvic floor are constantly tightened or contracted. This continuous contraction may result in pain and a series of discomfort. For a more detailed understanding, let’s break it down.
What is a Hypertonic Pelvic Floor?
The pelvic floor is a set of muscles situated at the bottom of the pelvic area. These muscles play a crucial role in body functions – bladder and bowel control, sexual function and childbirth. A hypertonic state of this muscle group means they are overactive and unable to relax.
This condition can affect both men and women, although it is more common in women. The overactivity can either be localized or generalized to the whole pelvic floor.
One key characteristic of hypertonic pelvic floor is chronic pelvic pain. This is due to the continuous tension of the muscles, leading to increased pressure in the pelvis. The pain can either be constant or intermittent and can greatly affect the quality of life of individuals suffering from it.
Functions such as urination, bowel movements, and sexual intercourse may become difficult or painful. This is because the constant tension prevents the muscles from stretching and relaxing as they should during these activities.
Many people mistake hypertonic pelvic floor for other similar conditions such as interstitial cystitis, pelvic inflammatory disease or endometriosis because they share similar symptoms. However, a hypertonic pelvic floor has a distinctive character – the chronic contraction of the pelvic floor muscles.
Despite its discomfort and potential impact on daily life and activities, a hypertonic pelvic floor is treatable. A range of treatments including physical therapy, lifestyle changes, and sometimes medication are available to help manage this condition.
Knowing the signs and seeking early treatment can prevent the condition from worsening and causing other complications. Understanding the factors that may trigger or worsen the condition can also help in managing a hypertonic pelvic floor. To do so, let’s first understand its causes.
What Causes a Hypertonic Pelvic Floor?
A hypertonic pelvic floor, also known as pelvic floor tension myalgia, occurs when the muscles in the pelvic floor become too tense or contracted. Various factors can cause this condition:
1. Physical and Emotional Stress: Both chronic physical and emotional stress can cause muscle tension, including in the pelvic floor.
2. Sitting for Prolonged Periods: People who sit for extended periods, such as office workers, often have tight pelvic floor muscles.
3. Surgically Induced Trauma: This includes hysterectomies, c-sections, and other pelvic surgeries that can cause scar tissue adhesions, resulting in a hypertonic pelvic floor.
4. Childbirth: The strain of childbirth can cause tearing, straining, and overall trauma to pelvic floor muscles, making them more prone to becoming hypertonic.
5. Pelvic Inflammatory Disease (PID): This disease can cause inflammation of the pelvic organs, causing chronic pain and tension in the pelvic floor.
6. Poor Postural Habits: Poor posture can put strain on the pelvic floor muscles, leading to hypertonicity.
7. High Impact Exercise: Activities such as running or jumping can put a lot of pressure on the pelvic area, potentially leading to a hypertonic pelvic floor.
8. Genetic Factors: Some people may be genetically predisposed to developing a hypertonic pelvic floor.
9. Problems With Bowel Movements: Chronic constipation, straining during bowel movements, and inflammatory bowel disease can lead to a hypertonic pelvic floor.
10. Hormonal Changes: Hormonal changes during the menstrual cycle can affect the pelvic floor muscles, causing them to contract.
Treatment usually involves pelvic floor physical therapy, lifestyle modifications, and treating any underlying pathological conditions.
How is Hypertonic Pelvic Floor Diagnosed?
A hypertonic pelvic floor is diagnosed by a medical professional such as a doctor or a physical therapist. Here are some methods commonly used:
1. Medical History: The healthcare provider will take a medical history, asking questions about symptoms, any recurrent urinary tract infections or conditions, childbirth history, surgical history, and bowel habits.
2. Physical Examination: This usually involves a manual exam of the pelvic floor muscles by a trained professional.
3. Biofeedback: In some cases, biofeedback devices can be used to help gauge muscle tone and control. These devices provide visual or auditory feedback to help one understand when their muscles are relaxed or contracted.
4. Ultrasound Imaging: In some cases, ultrasound imaging is used to visualize the muscles and surrounding structures in the pelvic region.
5. Cystoscopy or Sigmoidoscopy: In some cases, a cystoscope (a lighted instrument) is inserted into the urethra to view the bladder and evaluate any potential related issues. The same is done with a sigmoidoscope into the rectum to inspect the rectum and lower part of the colon.
6. Other Diagnostic Tests: Depending on the signs and symptoms, further investigations such as MRI, CT scan might be performed.
As with any medical condition, it is critical that the patient is truthful and forthcoming about their symptoms and history, as this information greatly aids in diagnosis.
What Are The Symptoms of Hypertonic Pelvic Floor?
The state of the hypertonic pelvic floor presents certain typical symptoms.
The foremost symptom is the unending discomfort or pain in the lower pelvic region. This pain might extend to the lower back and can vary in intensity from mild to severe.
Urinary symptoms are also prevalent in people with hypertonic pelvic floor. These might include painful urination, increased frequency of urination, and an urgent need to urinate.
Bowel discomfort, including constipation, straining during bowel movements, and feeling of incomplete evacuation are also characteristic symptoms of hypertonic pelvic floor.
For women, dyspareunia or pain during sexual intercourse, pain during menstrual periods, and difficulty using tampons can point towards hypertonic pelvic floor.
Other symptoms such as sexual dysfunction (in men), chronic prostatitis, rectal pain, unexplained hip or SI joint pain could also be present in cases of hypertonic pelvic floor.
What Are The Treatment Options for Hypertonic Pelvic Floor?
The choice of treatment for hypertonic pelvic floor is often dependent on the severity of the symptoms along with individual patient preferences.
Physical therapy is typically the first line of treatment. It includes techniques such as pelvic floor stretches, kegel exercises, biofeedback, and soft tissue massage to help relax the muscles of the pelvic floor.
Use of medication may be necessary for those experiencing severe pain or discomfort. Muscle relaxants, analgesics, and even some anti-depressants can be prescribed to reduce the symptoms.
Biofeedback is another form of therapy where electrical sensors are used to monitor bodily functions like muscle tension. With biofeedback, patients can learn to better control their pelvic floor muscles.
Surgery might also be a treatment option but it’s typically the last recourse when all other non-surgical treatments have failed to bring relief.
Dietary and lifestyle changes, including avoidance of triggers can also be beneficial in managing hypertonic pelvic floor, as we’ll next discuss in our subsequent sections.
How Does Physical Therapy Help Hypertonic Pelvic Floor?
Physical therapy often plays a crucial role in treating hypertonic pelvic floor.
The purpose of physical therapy in this context is to train the pelvic muscles to relax and contract appropriately. This is achieved through various exercises and techniques, usually performed under the guidance of a trained pelvic floor physical therapist.
These exercises include pelvic floor stretches, Kegels, and relaxation techniques, among others. These aim at relaxing the tense muscles, improving muscle strength and promoting proper muscle function.
Biofeedback is an integral part of physical therapy, helping patients gain control over their pelvic muscles. This involves the use of sensors to monitor muscle tension and provide real-time feedback, allowing patients to better understand their pelvic muscle behavior and manage them accordingly.
When consistently performed, these therapies can significantly improve the symptoms of hypertonic pelvic floor, making physical therapy an essential part of treatment.
Can a Hypertonic Pelvic Floor Lead To Other Complications?
Yes, if left untreated, hypertonic pelvic floor can manifest in more complex conditions.
Chronic pelvic pain is a common complication of untreated hypertonic pelvic floor. The constancy of this pain can affect quality of life significantly.
Sexual function can also be affected due to ongoing pain and discomfort. Discomfort during intercourse can lead to sexual dysfunction and strained relationships.
Urinary and bowel incontinence can also arise as a result of untimely relaxation and tension of the pelvic muscles. This unregulated muscle behavior can affect bladder and bowel movements.
Untreated pelvic floor tension can also result in prolapse of pelvic organs. This is a condition where the organs in the pelvic region like the uterus, bladder or rectum droop due to the weakening of the surrounding muscles and ligaments.
Therefore, early identification and treatment of hypertonic pelvic floor is crucial to prevent potential complications.
What Lifestyle Changes Can Help Manage Hypertonic Pelvic Floor?
People can make several lifestyle modifications to manage the symptoms of hypertonic pelvic floor.
Proper nutrition and hydration can assist in easing constipation and improving overall bowel health. Consuming a diet high in fiber can help soften stools and promote regular bowel movements, and drinking lots of water can further support this.
Avoid activities that strain the pelvic region, such as heavy lifting or long periods of sitting or standing. Taking regular breaks from such activities, changing positions, and incorporating gentle exercise like walking or stretching can be beneficial.
Managing stress is also important as it can trigger or worsen hypertonic pelvic floor symptoms. Relaxation techniques like yoga, meditation, and deep breathing can help reduce stress levels.
Finally, regular physical therapy can help maintain muscle flexibility and strength.
Can Hypertonic Pelvic Floor Be Prevented?
While there isn’t a surefire way to prevent hypertonic pelvic floor, certain measures can help reduce its risk.
Managing stress and anxiety through therapy or stress-relieving activities can prevent the unconscious tensioning of pelvic muscles.
Adequate toilet posture and habits can also contribute. For instance, not delaying the urge to urinate or defecate can reduce the strain exerted on the pelvic muscles.
Regular exercise, particularly exercises that target the pelvic muscles can keep them well-conditioned and less likely to adopt a chronic tension state.
Leading a balanced lifestyle, following a proper dietary regimen, maintaining hydration, and proactively managing weight can all play a role in preventing hypertonic pelvic floor.
Finally, seeking medical advice if symptoms arise can prevent the progression to a chronic state of hypertonic pelvic floor.
Difference Between Swedish and Deep Tissue Massage
Swedish and Deep Tissue are two popular types of massage therapies. While they may seem similar at first glance, there are key differences between the two. A Swedish massage is often thought of as a “standard” massage. Its primary goal is relaxation and improved circulation. The therapist uses a variety of techniques in a Swedish massage including stroking and gliding, kneading, rubbing, tapping or pounding, and vibration.
Deep tissue massage, on the other hand, is less about general relaxation and more about treating muscle pain and improving stiffness. It’s often used to treat specific problems, such as chronic muscle pain, injury rehabilitation, and the following conditions: Low back pain, Limited mobility, Recovery from injuries (e.g. whiplash, falls), Repetitive strain injury, such as carpal tunnel syndrome, Postural problems, Muscle tension in the hamstrings, glutes, IT band, legs, quadriceps, rhomboids, upper back.
While both massage styles can alleviate pain, they achieve this in different ways. Swedish massage focuses on improving circulation of blood and lymph and relaxing superficial muscles. Deep tissue massage focuses on connective tissue, and the goal is to release chronic muscle tension or knots.
Swedish and Deep Tissue Massage: How do the techniques differ?
The techniques used in Swedish and Deep Tissue massages vary significantly. Again, Swedish massage involves long, gentle strokes along with friction and tapping movements on the topmost layers of the muscles, combined with the movement of the joints.
With Deep Tissue Massage, the therapist applies stronger pressure and uses specialized techniques to reach the deeper layers of muscle and connective tissue. These techniques often involve slow, direct pressure or friction applied across the grain of the muscles.
When should you choose a Swedish massage over a Deep Tissue massage?
Choosing between a Swedish and a Deep Tissue massage often depends on what you want to get out of the session. If you’re primarily interested in relaxation and reducing muscle tension caused by daily activities like desk work, a Swedish massage may be the better choice.
It’s also often recommended for individuals who are new to massage, have a lot of tension, or are sensitive to pressure. Its gentle nature makes it a great first step into the world of massage, allowing individuals to experience the benefits without the intensity of deep tissue work.
When is a Deep Tissue Massage more beneficial than a Swedish massage?
Conversely, if you are coping with a specific issue, like chronic muscle pain, injury recovery, or rehabilitating from a sports injury, a Deep Tissue massage would likely be more beneficial. This type of massage aims to alleviate deep-seated tension, making it a good option for people with chronic pain or anyone experiencing muscle tightness or discomfort.
Deep tissue massages are also often a habitual part of an athlete’s regimen, as they can aid in performance, recovery, and injury prevention. They are advocated for their potential to treat various health conditions, ranging from fibromyalgia and hypertension to sciatica and tennis elbow.
Can Swedish and Deep Tissue Massage be combined for optimal results?
It is not uncommon for a massage session to combine elements of both Swedish and deep tissue massage. Many therapists will use Swedish massage as a foundation, and then integrate techniques from deep tissue massage to address specific pain or injury.
This combination can be particularly effective since Swedish techniques can warm up the muscle tissue, making it more pliable and ready for deeper work. After the deep tissue techniques, more Swedish massage could be used to soothe and settle the muscles.
What are some common misconceptions about Swedish and Deep Tissue Massage?
There are numerous misconceptions about both Swedish and Deep Tissue Massage. One common misconception is that deep tissue massage is simply a harder version of a Swedish massage. While the pressure is typically more intense in a deep tissue massage, its purpose is not to simply “go harder.” Instead, the goal is to reach, manipulate, and release tension in the deeper muscles and connective tissues.
Another misconception is that deep tissue massage should always hurt. While it’s true that the techniques used in a deep tissue massage can cause some discomfort, a good massage therapist will work within the client’s comfort level and utilize communication to ensure a beneficial and comfortable experience.
How does the intensity and pressure differ between Swedish and Deep Tissue Massage?
In a Swedish massage, the therapist uses lighter pressure and a variety of strokes including effleurage (gliding movements), petrissage (kneading), friction, vibrational, and percussion techniques. Swedish massage is more about broad techniques applied to the overall body with the main aim being to promote relaxation and improve blood circulation.
Deep tissue massage techniques are used to break up scar tissue and physically break down muscle “knots” or adhesions (bands of painful, rigid tissue) that can disrupt circulation and cause pain, limited range of motion, and inflammation. In deep tissue massage, there is a lot more focused pressure on specific areas and it can cause some discomfort.
What are the long-term benefits of each type of massage?
Both massages have different long-term benefits. Swedish massage is great for improving blood circulation, easing muscular strain, reducing emotional and physical stress, and promoting relaxation. Regular Swedish massage sessions have been found to decrease anxiety and improve energy levels.
On the other hand, deep tissue massage helps in managing chronic pain conditions, reducing blood pressure levels, breaking up old scar tissue, and promoting faster healing of injured muscular tissue. Regular sessions of deep tissue massage can substantially improve posture and support overall wellbeing and health.
What should one expect during and after a Swedish and a Deep Tissue Massage?
During a Swedish massage, the therapist lubricates the skin with massage oil and performs various massage strokes, including the basic techniques for a traditional Swedish massage: effleurage, petrissage, friction, tapotement, and vibration. These movements warm up the muscle tissue, releasing tension and gradually breaking up muscle “knots” or adhered tissues, called adhesions. Swedish massage promotes relaxation, among other health benefits.
During a deep tissue massage, a trained therapist delivers intense pressure through slow, deliberate strokes to target the inner layers of your muscles and connective tissues. This helps to break up scar tissue that forms following an injury and reduce tension in muscle and tissue.
After a Swedish massage, you should feel relaxed and rejuvenated, with any muscle tension significantly reduced. You may also notice improved circulation and flexibility.
After a Deep Tissue Massage, it’s not uncommon to experience some soreness for a few days following the treatment. This is similar to the discomfort many people experience after a heavy workout. Though, you should feel better and with less muscle tension within a day or two. Drinking plenty of water post-massage is also recommended to help flush out any toxins released from your muscles during the massage.
Car Accident Physical Therapy: a Patient Guide
Car accident physical therapy, also known as auto accident rehabilitation, is a specialized form of therapeutic intervention. It’s designed to reduce pain, restore body function, and help individuals return to their everyday activities following a car accident.
The human body responds to car trauma with inflammation and muscle rigidity, which can lead to restricted movement and discomfort. Physical therapy works to alleviate these reactions, improving and initiating the healing process.
Therapists can tailor unique treatment plans, adopting various techniques like joint mobilization, myofascial release, and therapeutic exercises. This personalized approach helps address issues such as acute pain, tissue swelling, and muscle weakness.
The intensity of therapy depends on the accident’s severity and the individual’s injuries. For some, therapy may focus on regaining flexibility and strength, while others might require more extensive rehabilitation, such as learning to walk again.
Modalities like heat therapy, cold therapy, or electrical stimulation are also part of car accident rehabilitation. They can help manage pain and speed up recovery by improving circulation and reducing inflammation.
Finally, physical therapists educate patients about self-care techniques that can be practiced at home. These exercises maintain progress made during therapy sessions and help prevent possible future injuries.
Aftercare is an essential component of car accident rehabilitation. It involves regular follow-ups to ensure patients sustain physical and emotional recovery. Therapists may adjust treatment plans based on individual progress and feedback.
All in all, car accident physical therapy is a holistic, patient-oriented approach to reignite individual healing potential. It goes beyond merely treating physical injuries to restoring overall health, wellness, and quality of life.
Initiation of Physical Therapy after a Car Accident
The timing to begin physical therapy after a car accident depends on the nature and extent of the injuries sustained. However, it’s typically advised to begin therapy as soon as possible, usually within a few days to a week post-accident.
Swift initiation of physical therapy can prevent the formation of scar tissue, which may lead to chronic pain and mobility issues. Early intervention also helps keep inflammation under control, which aids in speeding up the healing process.
Before starting therapy, a physical therapist will conduct a thorough assessment to determine the patient’s physical condition. This analysis consists of tests and observations to comprehend the range of motion, strength, balance, coordination, posture, and pain levels.
Based on this assessment, the therapist will devise an individualized treatment plan. This plan will outline the therapies to be employed and the treatment frequency and duration, and will also set short-term and long-term recovery goals.
It’s crucial to note that even minor accidents can lead to injuries that may not show symptoms immediately. Delayed treatment in such instances might result in further complications. Thus, even if the initial discomfort subsides, starting physical therapy can help detect and address these hidden injuries.
Persistence and regularity are significant factors while undergoing physical therapy; hence, the individual must remain committed to the process. Skipping sessions can disrupt progress and prolong the recovery timeline.
Patient’s compliance with home exercises, as directed by the therapist, is equally critical. Practicing these exercises between therapy sessions can accelerate recovery and prevent future discomfort.
Proactive communication with the therapist about pain, discomfort, and other symptoms helps in adjusting and optimizing the treatment plan. It ensures the therapy remains effective and aligned with the individual’s recovery goals.
Benefits of Car Accident Physical Therapy
Car accident physical therapy provides a plethora of benefits that contribute to faster and more efficient recovery. Here are some of the significant advantages:
-
- By employing different therapeutic techniques, physical therapy can alleviate pain and discomfort stemming from car accident injuries. Therapies like heat and cold therapy, joint and soft tissue mobilization, and electrotherapy can reduce pain and inflammation effectively.
- One of the most significant benefits of physical therapy is mobility restoration. Accidents often lead to a restricted range of motion due to stiffness and swelling. Therapists use specific stretches and strengthening exercises to help regain flexibility and movement.
- Physical therapy can also accelerate the body’s natural healing process. By improving blood circulation and reducing inflammation, the body can better heal the affected areas.
- By addressing physical pain and limitations, physical therapy indirectly aids in improving mental health. As the individual gains control over their body and experiences reduced pain, they often report decreased symptoms of anxiety, depression, and other mental afflictions related to their accident.
- Preventing long-term damage is another key benefit of undergoing physical therapy. By addressing injuries promptly, therapy may help prevent chronic issues that could appear months or even years after the accident.
- As therapists customize treatment plans to suit individual needs, patients receive personalized treatment plans. Such plans ensure that therapy addresses specific individual needs and injuries.
- Beyond immediate recovery, physical therapy also aims at building strength and resilience to prevent future injuries.
- Car Accident Physical Therapy also assists individuals in returning to their usual daily activities, including work, sports, and hobbies. This return to normalcy significantly aids the overall healing process.
- Physical therapists also educate patients about self-care and home exercises that can make a significant difference in recovery. Regular practice of these exercises helps sustain progress made during therapy sessions.
In essence, the benefits of physical therapy following a car accident extend beyond mere physical recovery. It provides a holistic healing approach by enhancing mental wellness, preventing long-term complications, and contributing to an improved quality of life in the long run.
Role of Physical Therapy in Car Accident Recovery
Physical therapy plays a vital role in a comprehensive recovery plan after a car accident, focusing on mitigating pain, restoring mobility, improving strength and flexibility, and accelerating the healing process.
Again, physical therapists conduct a thorough evaluation to identify the injuries and their impact. Post-evaluation, they develop customized treatment plans, detailing the kind of therapies, the number of sessions, and the expected recovery time frame.
One of the primary ways physical therapy aids car accident recovery is pain management. Therapies like ultrasound, TENS, and aqua therapy can significantly reduce pain and inflammation, resulting from musculoskeletal injuries.
Furthermore, physical therapists use specific mobilization techniques and exercises to restore range of motion. These exercises concentrate on relieving stiffness and enabling smoother, pain-free movements.
Strengthening exercises form a critical component of the recovery treatment plan. By building muscular strength — especially in injured areas — physical therapy contributes to faster healing and guards against further injuries.
Physical therapy is not just for immediate recovery; it is also about preparing the body for the future. Therapists teach patients how to perform exercises at home that help maintain strength, flexibility, and functionality.
Another crucial aspect of recovery that physical therapy impacts is the return to daily life activities. By gradually increasing the complexity of exercises, therapists help patients regain the ability to perform tasks independently, boosting their sense of autonomy and control.
Physical therapy also helps with stress management and emotional wellbeing. The process of healing and taking active steps towards recovery can significantly improve patients’ mental health, an often overlooked aspect of accident recovery.
Finally, physical therapists provide comprehensive education on self-care, posture correction, and injury prevention, essential for long-term health and wellbeing.
In essence, physical therapy takes a person-centered approach to car accident recovery, focused on individual needs and goals. It’s less about achieving a ‘standard’ recovery and more about enabling each patient to return to their life as comfortably and fully functional as possible.
Duration of Recovery with Car Accident Physical Therapy
The duration of recovery with car accident physical therapy depends on multiple factors such as the severity of the accident, the nature of the injuries, the patient’s age and health status, and their commitment to the therapy program.
Minor injuries such as sprains, strains, and whiplash might require a few weeks to a couple of months for recovery with regular physical therapy. During this period, the patient usually engages in gentle stretching, strengthening exercises, and modalities to control pain and inflammation.
More severe injuries like fractures or traumatic spine injuries, will necessitate a longer recovery duration. It can range from several months to over a year. This lengthier process might include both passive and active therapies, post-operative rehabilitation, and pain management techniques.
A critical element influencing the timeline is the patient’s adherence to the treatment plan. Regular attendance of therapy sessions and diligent execution of home exercise programs can expedite the recovery process.
Age and general health status also play significant roles in recovery duration. Older individuals or those with pre-existing health conditions usually take longer to heal than younger and healthier patients.
A crucial part of determining the recovery timeline is the initial assessment conducted by the physical therapist. It gives a rough estimate of the duration needed based on the injuries and the patient’s current physical condition.
Although the therapist provides an estimated timeframe, it’s essential to understand that each person’s healing journey is unique. Regular reassessments are performed during the treatment process to track progress and make suitable adjustments to the plan.
Pain duration can be a misleading determinant of recovery duration. Symptoms like pain and stiffness may disappear before the complete healing of the tissues. Physical therapy should continue until full restoration of function to prevent any chronic problems in the future.
In sum, a multitude of factors influence the recovery timeline with car accident physical therapy. Patience, consistency, and open communication with the therapist can contribute to a more effective and smoother recovery journey.
Physical Therapy and Pain Management after a Car Accident
A principal objective of car accident physical therapy is pain management. It serves to alleviate discomfort, promote healing, and mitigate reliance on pain medication.
Understanding pain in car accident injuries first involves recognizing the trauma-induced inflammation and swelling. Physical therapy offers techniques like cryotherapy (cold therapy) and thermotherapy (heat therapy) to reduce such inflammation, thus relieving pain.
Manual therapy, including joint mobilizations, massage, and myofascial release, is another effective method for pain management. By improving tissue mobility and blood circulation, these techniques aid in relieving pain and promoting healing.
Another modality employed in pain management is electrostimulation. Transcutaneous Electrical Nerve Stimulation (TENS) and Electrical Muscle Stimulation (EMS) can provide significant relief from acute and chronic pain.
Therapeutic exercises form the backbone of any physical therapy program, and they’re effective for pain management. Therapists design these exercises to enhance strength, flexibility, endurance, and overall function, thereby directly and indirectly helping in pain reduction.
Education on correct body mechanics and self-care exercises are also components of the pain management process. These techniques enable patients to manage their pain independently and prevent future injury or discomfort.
To further a patient’s comfort, therapists may employ special equipment, such as braces or orthotics. These resources provide support, align structures and help distribute forces evenly, reducing stress on painful areas.
It’s crucial to remember that pain is subjective and personal. A good therapist always validates a patient’s pain and resist comparing it with others. They adjust the therapy program based on the individual’s pain tolerance and feedback.
Comprehensive pain management in physical therapy also addresses psychological aspects. Therapists often integrate relaxation techniques, mindfulness, cognitive behavioural therapy, or refer to mental health professionals, recognizing the interlinkage of pain and psychological well-being.
In essence, car accident physical therapy offers a multidimensional approach to pain management. It combines several modalities for pain relief, aims to sustain pain reduction through strength and flexibility training, and empowers patients to take charge of their pain management journey.
Expectations from First Physical Therapy Session after a Car Accident
The first physical therapy session post a car accident forms the foundation of the recovery journey. It involves assessments, goal setting, initial treatments, and introductions to exercises. Here’s what to expect:
To start with, the physical therapist will discuss the accident’s details, medical history, symptoms, pain levels, and your overall health. An open honest discussion about expectations and apprehensions will also occur.
Next, the therapist will perform a comprehensive clinical evaluation. This includes but isn’t limited to observing posture, assessing range of movement, evaluating strength, testing reflexes, and identifying pain points.
Based on the information gathered, the therapist will develop an individualized treatment plan. It consists of the types of therapies to be used, the frequency of sessions, and the overall objectives of the therapy.
Initial treatment may commence from the first session itself. It would typically involve methods to manage pain, reduce swelling and promote relaxation. This might involve modalities like hot/cold therapies, ultrasound, or mild electric currents.
You will be introduced to some gentle exercises, postures, and movements that help to alleviate pain, reduce stiffness, and improve range. These exercises will provide a preview of what subsequent therapy will include.
In the first session, the therapist may discuss the incorporation of home exercises into your routine. They will guide you through these exercises and provide documentation to ensure you can perform them correctly and safely.
The therapist will also educate you about what to expect during and after therapy sessions. A critical part of this education is understanding that it’s normal to feel a little discomfort during and after exercises, but acute, lasting pain is not.
You will be informed of how to manage post-therapy soreness and the measures to take if you experience severe or prolonged pain.
The first session is also where you realize that your active participation is integral to the therapy’s success. You’re encouraged to communicate openly about your pain, apprehensions, and changes in your condition, without any hesitation.
In a nutshell, the first physical therapy session post car accident sets the tone for your recovery journey. It forms an integral place for comprehensive assessments, baseline treatment, education, and sets the stage for a collaborative patient-therapist relationship aimed at goal-oriented recovery.
Value of Physical Therapy in Mental and Emotional Recovery after a Car Accident
Mental and emotional recovery after a car accident tends to be downplayed compared to physical recovery. However, with increasing realization of the interconnectedness of physical and mental health, physical therapy is acknowledging its role in addressing the psychological aftermath of a car accident.
Experiencing a car accident can leave survivors with emotional and mental trauma, including anxiety, depression, and in some cases, post-traumatic stress disorder (PTSD). Undertaking physical therapy can indirectly contribute to managing such conditions.
A routine, such as regular physical therapy appointments, can be therapeutic for accident survivors. It brings a semblance of order and predictability in the upheaval post-accident, which offers emotional relief and bolsters mental stability.
Physical exercises release endorphins, known as “feel-good” hormones, which boost mood and counteract feelings of depression. Hence, the active engagement in exercises during therapy can induce a positive mental state.
Relaxation techniques taught by physical therapists, including deep breathing and mindfulness, are potent tools to manage anxious thoughts and induce calmness. By reducing physiological stress symptoms, these techniques can help achieve emotional balance.
The relationship between pain and mental distress is bidirectional, meaning that reducing pain through physical therapy can lead to an improved mental state, and vice versa.
Ultimately, car accident physical therapy adopts a holistic approach to care, acknowledging that mental and emotional health influences the recovery process. Physical therapy becomes a space not only for physical healing but also for survivors to regain their sense of self, confidence, and positivity.
Are you struggling after a car accident and looking for physical therapy?
Things to Avoid with Degenerative Disc Disease
What types of physical activities should I avoid with Degenerative Disc Disease?
It’s crucial to note that while regular moderate exercise is beneficial for most people suffering from degenerative disc disease (DDD), not every physical activity is recommended. Some activities can place an excessive strain on the back and spine, leading to increased pain and potential further damage to the discs. It’s important to understand and consider these factors while engaging in physical activity.
High-impact activities like running and basketball that jar the spine should be preferably avoided as they increase pressure on the intervertebral discs, leading to exacerbation of DDD symptoms. Similarly, heavy weight lifting, characterized by the tremendous amount of stress it places on the spine, is not recommended for those suffering from DDD. Also, bending and twisting movements, particularly during lifting, should be eschewed as these motions amplify pressure on the spine and may result in further injury.
Low-impact activities like walking, swimming, or yoga are beneficial for individuals with DDD. These exercises gently stretch and strengthen the back muscles without causing harm. However, it’s vital to avoid overdoing these exercises to prevent muscle fatigue and instability. Furthermore, it is advisable to immediately halt any exercise or movement that induces pain, as pain serves as a warning from our bodies that something isn’t right.
Extended periods of sitting or standing can be detrimental and thus should be avoided if possible. If your job necessitates you to remain in a single spot for long stretches, make sure to take frequent breaks to move around. Moreover, maintaining an accurate posture while sitting and standing can help to alleviate stress on your spine. Slumping or slouching should be consciously avoided.
Lastly, it is crucial to avoid lifting heavy objects when tired or distracted, as this could lead to improper body mechanics. Moreover, be extra cautious on stairs and slippery surfaces, as falls can cause serious damage to an already sensitive back. Remember, it’s crucial to prioritize safety and comfort when dealing with DDD, and these guidelines will significantly help in managing this condition.
Always consult with your doctor or a physical therapist before starting a new exercise regimen. They can suggest appropriate and safe exercises for your condition and teach you how to perform the movements correctly to avoid injuries.
Are there certain types of food I should avoid with Degenerative Disc Disease?
Just like with other diseases, certain foods may induce inflammation, leading to amplified pain in individuals with degenerative disc disease. Here is a discussion of the problematic foods:
1. Processed foods often contain high levels of sodium and unhealthy fats, leading to increased inflammation levels.
2. Sugary foods can trigger an inflammatory response in your body, worsening DDD symptoms.
3. Fast foods, while convenient, are often high in saturated fats and can intensify inflammation.
4. Alcohol doesn’t offer any nutritional benefit and can contribute to inflammation and dehydration. This lack of fluid may lead to a further degeneration of spinal discs.
5. Caffeine can also act as a diuretic, leading to dehydration and aggravating back pain.
6. Red meat is known to cause an inflammatory response in the body.
7. Dairy products may lead to inflammation, especially in individuals who are lactose intolerant.
8. Gluten has been associated with inflammation, particularly for those with a gluten intolerance or allergy.
9. Foods high in trans fats, like baked goods and fried foods, can increase inflammation.
10. Aspartame, often found in diet sodas and sugar-free candies, may increase pain and inflammation.
Knowing what to avoid is only half the picture. Eating a balanced diet, staying properly hydrated, and maintaining a healthy weight also helps manage degenerative disc disease.
Should I avoid alcohol and tobacco with Degenerative Disc Disease?
Degenerative disc disease (DDD) is significantly impacted by our lifestyle choices. Two particularly detrimental habits affecting the condition are consumption of alcohol and tobacco.
Alcohol consumption can negatively impact DDD in several ways. Firstly, alcohol leads to dehydration, making the discs in the spine dry and brittle. This causes exacerbated pain levels and increased disability. Chronic alcohol use also disrupts proper sleep schedules and patterns. Sleep is crucial for the body’s recovery and restoration processes; disruption to sleep can therefore hinder the healing and restoration of spinal discs.
Furthermore, alcohol consumption can contribute to weight gain and obesity. This additional weight puts unnecessary strain on the back, further deteriorating the condition of the spinal discs. Meanwhile, regular consumption of alcohol can interfere with the body’s ability to absorb and use nutrients vital for bone health. This can result in a reduction in bone density and an increased risk of fractures.
Moreover, heavy drinking enhances the risk of accidental falls and injuries. Any injury to the back could potentially worsen an existing DDD condition. Meanwhile, smoking habits also contribute to a worsening of DDD. Smoking effectively decreases blood flow, starving the spinal tissues of vital nutrients and encouraging the spinal discs to degenerate more swiftly.
Nicotine, a compound present in tobacco, can cause a loss of flexibility and strength in the spinal discs. This leads to an increased risk of injury to the spinal cord. Additionally, smoking can provoke coughing fits which exert pressure within the chest area and throughout the spine, adding undue stress on the spinal cord. It also impairs the body’s healing process, dealing a blow in cases of injury or post-surgery recovery. Furthermore, smoking can lower the effects of treatment – so much so that most surgeons hesitate to perform certain procedures on smokers due to the high complication rate.
Consequently, avoiding alcohol and tobacco consumption can significantly enhance an individual’s overall health. Additionally, these lifestyle adjustments can slow down the progression of degenerative disc disease, leading to an improvement in the quality of life for individuals suffering from DDD.
Is incorrect posture an issue with DDD and how can I avoid it?
Posture plays a vital role when it comes to managing degenerative disc disease (DDD). Maintaining incorrect posture exerts excessive stress and pressure on our spine, which can accelerate disc degeneration. Therefore, it’s essential to pay attentive care to our postures both in standing and sitting positions. By adopting proper posture, we can distribute our body’s weight evenly, reducing the strain on the back and delaying the progression of DDD.
Shoe choices also contribute to maintaining correct posture. High heels or shoes that lack adequate support compromise our spinal balance and should be avoided. While engaged in activities such as working or studying, it is crucial to ensure that our seats let our feet touch the ground and our computer screens are at eye level. This stance helps to prevent unnecessary inclinations and reduces the strain on our neck and back.
Forward bending of the neck and hunching of shoulders can exacerbate the rapid degeneration of the spine, so they should be avoided as much as possible. It’s essential to take breaks in between work or study, avoiding sitting or standing for extended durations. Continuously being in one position leads to additional pressure on the spinal discs.
Investing in adequate quality chairs and mattresses is another smart choice. These provide the necessary support for our backs and aid in maintaining a neutral spine position. Moreover, regular activities such as yoga and exercises targeted at strengthening the abs and back muscles improve our body posture and supply better support to our spine.
Guidance from physical therapists can be beneficial as they can recommend specific exercises aimed at rectifying posture and alleviating the harsh symptoms of DDD. Lastly, being mindful of your posture during various activities like walking, lifting, and sitting can significantly aid in managing DDD. Ultimately, by maintaining proper posture, we can slow down the progression of degenerative disc disease significantly.
Are there any household chores that are not recommended for Degenerative Disc Disease patients?
Many daily chores that individuals encounter can exacerbate the symptoms of degenerative disc disease. Tasks like continuous bending and lifting, such as vacuuming or hauling heavy laundry baskets can put a strain on the back. Therefore, it’s crucial to modify how these activities are performed to protect the spine.
Similarly, chores that require you to maintain the same position for a long period, like ironing or chopping vegetables, need to be avoided, or at least, break periods in between should be considered. A beneficial tip is to bend knees and squat when picking something from the floor, instead of bending over from the waist; this can aid in protecting your back from strain and injury. Moreover, tasks that inherently require torso twisting, like sweeping or mopping, need to be done cautiously. During such chores, attempt to keep your hips and shoulders aligned as much as possible to prevent symptoms from flaring up.
Another essential factor to consider is balance. Carrying heavy items on one side of the body should be avoided, splitting the weight evenly between both sides instead. When handling tasks like weeding or mowing grass, you should always be mindful of your posture and take frequent breaks to protect your back from undue strain. Even while sitting and working on a computer, attention to sitting posture is crucial. Ensure that your feet touch the ground and your screen is at an eye-level position.
Whenever possible, try and utilize tools or devices that lessen the burden on your back. These may include an ergonomic chair or an adjustable bed. During cooking, avoid lifting heavy pots; using lighter cookware or shifting the pot off heat before lifting could prevent excessive strain on your back. Further, while doing dishes, care should be taken to avoid tipping your head downward for extensive periods as this can strain your neck and upper back.
With careful attention to how daily tasks and chores are performed, individuals with degenerative disc disease can manage their symptoms and slow the progression of the disease.
How does drastic climate change impact Degenerative Disc Disease?
Climate changes and weather fluctuations have a significant impact on individuals with degenerative disc disease (DDD). Some people with this condition may experience worsening of their symptoms in certain weather conditions, requiring tactical approaches to manage and mitigate discomfort.
Cold and damp weather tends to stiffen the joints, leading to increased pain for some individuals with DDD. Extreme temperature changes also pose a challenge as they can affect the body’s ability to adapt and possibly lead to increased discomfort. It is prudent to stay warm in such weather conditions to alleviate these symptoms. On the other hand, during exceptionally hot days, DDD patients may experience heightened inflammation, which triggers more pain. This can be mitigated by staying in a cool environment and ensuring hydration.
Changes in barometric pressure often occur with weather changes and can instigate increased pain in certain individuals. One helpful strategy is to monitor these fluctuations and plan activities accordingly. Additionally, high humidity levels can exacerbate symptoms for some people. This can be alleviated by ensuring the living environment is comfortable, preferably with air conditioning.
Pleasant weather often invites increased physical activity which might inadvertently incite a flare-up in DDD symptoms. It’s therefore crucial to maintain a moderate level of physical activity and pace it regular to avoid any adverse effects. Similarly, seasonal shifts, especially from warm to cold weather, can worsen symptoms. Warm clothing and heat patches can be of great help to provide warmth and relief during colder seasons.
Winters are often associated with reduced sunlight, leading to low levels of vitamin D3, crucial for bone health. Regular intake of D3 supplements during this time might alleviate DDD symptoms. It’s also essential to keep the body hydrated and adhere to a balanced diet to better equip it to handle these weather changes.
Finally, establishing regular check-ins with a healthcare provider can play a pivotal role in effectively managing symptoms in sync with the changing seasons. To sum up, managing DDD is inherently about understanding and adapting to weather changes and taking the appropriate steps during dramatic climate shifts.
Do weightlifting and high-impact sports impact Degenerative Disc Disease, and should they be avoided?
Sports and exercise have immense benefits for our physical health and mental wellbeing. Yet, those dealing with degenerative disc disease (DDD) should proceed with caution when partaking in high-impact sports and weightlifting due to the potential adverse effects. High-impact activities such as football, soccer, and tennis involve a lot of running, jumping, and sudden directional changes. These movements put extreme strain on the back and spine, exacerbating DDD symptoms.
Similarly, weightlifting, especially if done with incorrect form and technique, places considerable pressure on the back and can lead to further disc deterioration. Moreover, activities involving repetitive twisting and turning place an excessive strain on the discs, leading to potential injury and the acceleration of degenerative changes in already damaged discs.
Participating in intensive training regimes without appropriate rest intervals also poses risks. Working the back muscles to exhaustion can increase spinal stress. Further, high-intensity workouts, when conducted without the necessary warm-up or cool-down sessions, often result in muscle stiffness and may amplify the discomfort associated with DDD.
Overloading the spine is another common danger in weightlifting. Carrying heavy weights on one’s shoulders or back should be avoided to prevent additional injury. Ignoring pain during exercise is detrimental. Pain during any activity should be regarded as an alarm bell signaling potential harm to the body.
Succumbing to the competitive nature of sports and pushing past physical limitations can also increase the risk of injuries and may worsen DDD symptoms. Similarly, accelerating the intensity or duration of workouts too quickly can have adverse effects on DDD. Gradually increasing activity levels is essential.
Before commencing weightlifting or any high-impact sports, a medical checkup is advisable. Healthcare professionals or physical therapists can offer advice on suitable exercises and provide guidelines on what activities to avoid. A well-considered exercise regimen composed of lower impact activities and correct techniques, carried out at a thoughtful pace, will enhance strength, flexibility, and assist with pain management. This strategic approach will enhance wellbeing without causing further damage to degenerative spinal discs.
Are certain sleeping positions bad for Degenerative Disc Disease?
Sleep and efficient rest are fundamental to healing and recovery, especially for individuals suffering from degenerative disc disease. Haphazard sleeping positions can worsen discomfort and impede recovery. Certain sleeping postures and considerations can minimize pain and bolster the healing process.
Sleeping on your stomach applies unnecessary stress on your spine and can worsen disc degeneration, so it’s advisable to avoid this posture. On the contrary, adopting a fetal position whilst sleeping might help in opening the spaces between the vertebrae. Using a pillow between the knees will ensure optimal spinal alignment and lessen pressure on the hips for side sleepers.
When you prefer sleeping on your back, utilizing a pillow under your knees can uphold the natural curve of the spine and offer relief. However, excessive use of pillows or very high pillows might lead to a forward positioning of the neck, which should be circumvented. Equally crucial is finding the right mattress; a model that maintains the spine’s natural curve and conforms to the heaviest body parts should be the aim.
If side-sleeping is preferable, alternating sides regularly can avert muscle imbalance. Use props like body pillows providing added support for the utmost comfort. Adjusting your bed’s design, for instance, raising the head or using an adjustable bed, could enhance symptom management. It is wise to avoid any posture or movement that has previously led to sharp pains or discomfort.
Strain on the neck can happen from habits like reading or using a mobile device while lying down. Employing an eye-level book or device stand can alleviate this problem considerably. Regular consultation with healthcare professionals about the preferred sleep posture can yield personalized advice. Good sleeping habits can substantially enhance the quality of life for those battling degenerative disc disease, making the effort to master them an investment in wellbeing.
Can some medications aggravate Degenerative Disc Disease that I should avoid?
Certain medications, though useful in treating certain conditions, can potentially increase the severity of the symptoms for those suffering from degenerative disc disease. Careful attention needs to be paid to these medications and a comprehensive understanding of their side effects or negative impacts is necessary.
Non-steroidal anti-inflammatory drugs, more commonly referred to as NSAIDs, can lead to serious health implications like gastrointestinal damage and kidney problems if used for a prolonged period. This could potentially reduce a person’s overall health and resilience. In a similar way, certain antidepressants can pose different threats. They may cause dry mouth, constipation, and urinary retention. This places additional strain on the body and can potentially worsen the symptoms of degenerative disc disease.
Moreover, the long-term use of corticosteroids could prove to be risky for those with this condition. Extended use can actually result in a person developing osteoporosis, a condition which those with degenerative disc disease are already at a higher risk for. Similarly, certain types of blood thinners run the risk of causing internal bleeding or haematomas. This could result in unnecessary pressure being put on the spine.
Additional medications to be aware of are bone-targeting medicines that are often used in cases of metastatic cancer. These can often cause severe back pain. Furthermore, certain types of antibiotics may interact negatively with degenerative disc disease. This is especially true for patients who have a similar autoimmune disease.
Even commonly used medications can pose a risk. Painkillers could potentially lead to dependency and increased tolerance, requiring higher doses over time. It is also essential to maintain a proper balance in consuming vitamins and minerals, as excessive consumption from supplements may lead to toxicity. Even over-the-counter medications should be taken with caution and moderation to avoid any potential negative impacts.
Lastly, before starting any new medication, it’s imperative to consult with a doctor. Being vigilant and informed concerning these aspects can contribute significantly to better healthcare and improved outcomes for patients dealing with degenerative disc disease.
Are you struggling with Degenerative Disc Disease?
Ball of Foot Pain: a Guide to Causes
Why Does the Ball of My Foot Hurt?
The ball of your foot, the pad just behind your toes, is vulnerable to different injuries and conditions which can result in discomfort or pain. It’s the area that bears the maximum weight and force when you walk, run or jump.
Poorly fitting shoes or high heels can put extra pressure on the ball of your foot, leading to pain. Sports or physical activities that involve running or jumping can also cause stress in this area.
Certain foot shapes, such as a high arch or flat feet, can contribute to an uneven weight distribution, causing pressure on the ball of your foot. This is further exacerbated if you’re overweight, as extra weight can strain the ball of your foot.
Your pain could be from metatarsalgia, an inflammation in the ball of your foot. In older adults, the fat pad in the foot may thin out, decreasing the padding and increasing the sensitivity of the ball of your foot.
Conditions like arthritis, diabetes, or a Morton’s neuroma (a non-cancerous growth on a nerve) can also cause pain in this area. Likewise, the ball of foot pain could be due to a bunion, a bony bump that forms on the joint base of your big toe, leading to pain and discomfort.
What are Possible Causes of Ball of Foot Pain?
Several conditions and factors can cause pain in the ball of the foot:
- Metatarsalgia: This condition occurs when the metatarsal bones, located in the ball of the foot, are inflamed.
- Neuroma: Known as Morton’s Neuroma, this condition involves a nerve in the foot being pinched or irritated.
- Sesamoiditis: This condition is either inflammation or a fracture of the sesamoid bones in the ball of the foot.
- Bunions or Hammertoes: These are foot deformities that place extra stress on the ball of the foot.
- Obesity: This involves excess weight which can put additional stress on the bones, muscles, and ligaments in the feet.
- Poorly Fitted Shoes: Shoes that are too narrow, have high heels, or lack enough padding can cause foot pain.
- High Impact Activities: Sports or physical activities that involve running and jumping can increase pressure on the ball of the foot.
- Aging: The natural fat pad on the feet can thin out as one ages, potentially causing pain and discomfort.
- Diseases: Conditions like diabetes, arthritis, or other inflammatory diseases can lead to foot pain.
How Do I Get Rid of Pain in the Ball of My Foot?
There are several ways to alleviate pain in the ball of your foot, many of which can be done at home:
- Rest your feet and avoid activities that cause your foot pain.
- Apply an ice pack to the painful area for 15 minutes at a time to reduce inflammation.
- Wear shoes with adequate arch support and a wide toe box.
- Use over-the-counter pain relievers and anti-inflammatory drugs to manage pain and swelling.
- Apply a foot pad to the affected area to help distribute weight more evenly.
- Perform stretching exercises to help strengthen and stretch the muscles in your feet.
If your pain persists or worsens over time, it’s crucial to seek medical attention. Depending on your specific case, a healthcare professional may recommend physical therapy, orthotic devices, steroid injections, or in extreme cases, surgery.
What Home Remedies can Alleviate Ball of Foot Pain?
Simple home remedies can often help manage or even alleviate ball of foot pain:
- Ice: Apply an ice pack wrapped in a cloth to the affected area for up to 15 minutes, several times a day to minimize inflammation.
- Elevation: Elevate your foot to help reduce swelling and relieve pain.
- Rest: Avoid activities that put pressure on your foot until the pain improves.
- Pain Relief Medications: Use over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen to reduce pain and swelling.
- Foot Exercises: Strengthening and stretching exercises can help increase flexibility and reduce pain.
- Proper Footwear: Wear shoes with a low to moderate heel, a wide toe box, and good arch support to help alleviate pain.
Remember that while these remedies can provide temporary relief, it’s crucial to tackle the underlying cause of your pain. If your pain persists, schedule a consultation with a healthcare professional like a physiotherapist.
Can Incorrect Footwear Cause Pain in the Ball of My Foot?
Yes, wearing shoes that don’t fit properly or don’t provide enough support can contribute to pain in the ball of your foot. High heels, for example, put a lot of pressure on the ball of your foot, which can lead to pain and other foot problems like bunions, hammertoes, and metatarsalgia.
On the other hand, footwear that’s too loose can cause your foot to slide forward while you’re walking, again, putting excessive pressure on the ball of your foot and leading to pain.
Shoes with thin soles or lack of cushioning won’t adequately absorb shock, increasing the stress on your feet. This not only causes pain, but it could also lead to or worsen conditions like neuromas, sesamoiditis, or stress fractures.
Finally, if your shoes lack good arch support, they can overwork your plantar fascia (the band of tissue that runs along the bottom of your foot), resulting in discomfort or pain.
How Can I Prevent Ball of Foot Pain?
One method to prevent or minimize foot pain is by focusing on your footwear. Choose shoes that not only fit well, but also provide proper arch support and have sufficient room in the toe box. Shoes with cushioned soles and a moderate heel height can further contribute to keeping your feet comfortable and pain-free.
Another critical factor in preventing foot pain is maintaining a healthy weight. Bearing extra weight increases the pressure on your feet, which can lead to discomfort or pain. Similarly, it can be helpful to adjust your physical activities to reduce the stress on your feet. Incorporating low-impact exercises such as swimming or cycling can help in achieving this.
Additionally, regular foot exercises that aim at stretching and strengthening your foot muscles can contribute to pain prevention. Alongside regular foot care, the use of shoe inserts or pads can alleviate pressure on the feet and provide extra cushioning for added comfort. Finally, it’s important to listen to your body cues. If your feet start hurting during activities, taking a break and allowing them to rest can prevent further discomfort.
What Are Good Foot Exercises to Alleviate Ball of Foot Pain?
Gentle exercises that stretch and strengthen the muscles of your feet can prove beneficial when looking to alleviate and prevent ball of foot pain. Among these exercises is the Toe Raises. The exercise involves sitting down and placing the affected foot flat on the floor. Then, you lift the toes while making sure the heel remains grounded. After a pause, you lower the foot down and repeat the exercise.
Additionally, the Marble Pick-Ups can be an efficient exercise. This exercise entails placing a few marbles on the floor and using your toes to pick these up and put them in a bowl, effectively stretching and strengthening the muscles in your feet. Further, the Towel Pulls exercise has demonstrated effectiveness. To do it, place a small towel on the floor, put your foot on the towel, and try to pull the towel towards you using your toes and while maintaining your heel on the floor.
Lastly, the Calf Stretch exercise should be considered. To perform this exercise, stand in front of a sturdy piece of furniture or a wall, bend one of your legs, and keep the other at the back and straight. Push your hands against the wall or furniture, press down on the heel of your back foot, and continue until you feel a stretch in your calf muscle. These exercises are beneficial in both treating and preventing foot pain.
When Should I Seek Medical Advice for Ball of Foot Pain?
If your ball of foot pain persists despite home remedies, or if it’s severe or accompanied by swelling or discoloration, you should seek medical help.
Your doctor might examine your foot and ask about your symptoms, physical activity, and footwear. They might also request imaging tests, such as X-rays or ultrasounds, to visualize your foot’s structure and identify any abnormalities.
Your healthcare provider might recommend different treatments based on your diagnosis, including physiotherapy, prescription medication, orthotic devices, or in severe cases, surgical intervention.
Can Orthotic Insoles Help Manage Foot pain?
Orthotic insoles can indeed help if you’re experiencing pain in the ball of your foot. These are devices made to align the foot and ankle into an anatomically efficient position.
Custom orthotics are molded to the contours of your foot and help to distribute weight evenly across your foot, reduce pressure on your pain points, provide cushioning for your feet, and correct your gait.
If you think you would benefit from orthotics, you should consult a healthcare professional like a podiatrist or a physiotherapist who can assess your condition and suggest the best plan for you.
Can Conditions like Arthritis Cause Pain in the Ball of My Foot?
Certain medical conditions, such as arthritis, could indeed cause pain in the ball of your foot. Osteoarthritis, for example, could affect the joints in your foot, including those located in the ball of your foot, causing pain.
Rheumatoid arthritis, an autoimmune type of arthritis, could also lead to foot pain. This condition can cause an inflammation of the joints in the foot, including the ball of the foot.
Another condition called gout, which is a form of arthritis, happens when uric acid crystals accumulate in a joint, leading to severe pain and swelling. The big toe is often affected, but other areas, including the ball of the foot, can also experience gout attacks.
If you suspect that arthritis might be causing your foot pain, it’s a good idea to consult a healthcare professional for diagnosis and treatment options.
Are you struggling with pain in the ball of your foot?
Neck Pain from Sleeping
Neck hurts after sleeping: what are the most common causes?
Neck pain after sleeping is not an uncommon experience for many individuals. It is often caused by a variety of factors. One of the most prevalent reasons is inappropriate sleeping positions. If your neck is twisted or bent too much, it can result in muscle strains and tension the next morning.
Pillows can also play a significant role in causing neck pain. A pillow that is too high or too soft might not provide your neck with the proper support it needs, leading to discomfort. Investing in a good quality mattress and maintaining its suitability over time is equally important. A sagging mattress can lead to poor sleeping posture, inevitably causing neck pain.
Stress is another significant contributor to neck pain after sleeping. People under high stress often have a lower pain threshold and tenser muscles, leading to neck pain. Medical conditions such as arthritis, nerve compression, and diseases of the spine may also cause neck pain post sleep. Unconscious movements during sleep could contribute to neck pain. If you tend to roll or move a lot during your sleep, it might lead to awkward neck positions, causing discomfort.
Sometimes, unusual activities or exercises performed the previous day can also cause neck pain in the morning. Activities that strain the neck muscles like heavy lifting can lead to inflammation and neck pain after sleep.
Lastly, aging could influence the experience of neck pain after sleeping. As one grows older, they are more susceptible to muscle strain and joint wear and tear, leading to frequent experiences of neck pain.
Thus, the causes for neck pain after sleeping are diverse, from incorrect sleeping positions and subpar pillows or mattresses, to stress, medical ailments, unconscious movements in sleep, strenuous activities, and the natural course of aging. Knowing these causes can help address the pain accurately and effectively.
Neck pain from sleeping wrong: what are the symptoms?
The experience of neck pain may vary between individuals and can be associated with a number of symptoms. Here, we identify the common symptoms associated with neck pain resulting from sleeping wrong.
Feeling a sharp or stabbing pain in the neck area is a common symptom. This may be localized to one area or diffuse across the neck. Sometimes, the pain may not be localized, but spread to nearby areas like the shoulders or the base of the skull. This pain could be continuous, or it may worsen with certain movements or activities.
Muscle spasms and tightness in the neck can be another symptom. You might find it difficult to move your neck, especially towards the side that hurts. Some people may also experience a dull ache or soreness in their neck, shoulders, or upper back. This pain could be persistent or it may come and go. Headaches often accompany neck pain. This is especially true if the neck pain is towards the back of the neck or is due to tension or stress.
In some cases, people may experience numbness or tingling sensations. These could be felt in the neck, shoulders, arms or hands and is usually a sign of nerve irritation. Difficulty in lifting objects or gripping things can also be a sign of neck pain resulting from sleep. This usually happens when the pain radiates down into your arms.
In rare cases, people might experience symptoms like nausea, fatigue, dizziness, or blurred vision along with their neck pain. These symptoms are not typically associated with neck pain from sleeping wrong and could be indicative of a more serious condition.
Symptoms of neck pain from sleeping wrong might interfere with daily activities and can severely affect quality of life. Appropriate identification of symptoms can aid in the right treatment and prevention of further pain.
How can neck pain from sleeping be prevented?
Preventing neck pain from sleeping involves various factors such as maintaining good sleep hygiene, choosing the right pillow and mattress, and practicing proper body mechanics.
- Maintaining a proper sleeping position can help prevent neck pain. The ideal positions include lying on your back with a pillow to support the natural curve of your neck or lying on your side with a pillow that is just high enough to keep your neck aligned with the rest of your body. Avoid sleeping on your stomach since it tends to twist the neck.
- Choose a supportive pillow that is tailored to your specific requirements. The pillow should maintain a height of about 4 to 6 inches and should support your neck and head while aligning with your spine. The pillow’s filling should be memory foam or polyester filling for optimal firmness and flexibility.
- Invest in a good quality mattress that provides support to all parts of your body. The mattress should be firm enough to support your body while conforming to your body’s curves.
- Ensure to maintain good posture throughout the day, as poor daytime posture can set the stage for nighttime problems. Avoid prolonged neck bending while working, reading or using your phone.
- Regular exercise that incorporates stretching and strengthening exercises can help maintain flexibility and range of motion in your neck, which can prevent neck pain during sleep.
- Practice stress management techniques like meditation, deep breathing, and progressive muscle relaxation, as high stress levels can increase muscular tension and lead to neck pain.
- Avoid heavy physical activity or unusual exercises before bedtime as it can strain your neck muscles.
- Regular check-ups and consultations with a chiropractor or a physical therapist can help in maintaining good neck health.
With the right measures taken, it is entirely possible to prevent neck pain from sleeping wrong, providing for a restful and refreshing sleep.
What sleeping positions are recommended to avoid neck pain?
When we sleep, our bodies go through several cycles of recovery and rejuvenation. During these times, it’s important to maintain a position that supports our spine’s natural alignment. Sleeping on your back or side is usually recommended to avoid neck pain. These positions help keep your neck neutral and prevent any unnatural bending or twisting. Moreover, a proper pillow and mattress can be extremely beneficial in further aiding this alignment.
A good pillow should follow the natural curve of your neck, not too high or too low, giving your neck the right amount of support.
When should I see a doctor for neck pain resulting from sleep?
Many of us experience mild neck pain from time to time, but if your neck pain persists for more than a week, it may be time to consult a physician. It could be interfering with your day-to-day activities and potentially indicating a more serious condition.
Symptoms like severe headache, numbness, weakness, or tingling sensations in your hands or arms could be associated with neck issues and should not be overlooked. And certainly, if the pain started after a traumatic event like an accident or fall, it’s paramount to immediately seek medical attention.
Are there any home remedies for treating neck pain after sleeping?
Home remedies for neck pain can be your first line of defense. Applying a heating pad to the affected area can loosen up the tight muscles, and stretching and strengthening exercises can help restore flexibility and resilience in neck muscles. Over-the-counter pain-relievers can also provide temporary relief.
Moreover, improving your sleep habits can go a long way in preventing recurring neck pain. This could mean setting regular sleep hours, selecting a suitable pillow and mattress that offer good support, and ensuring your sleeping posture contributes to the neutral alignment of your neck.
Is there a correlation between neck pain and specific types of pillows or mattresses?
Yes, there is a significant correlation between neck pain and the use of certain types of pillows and mattresses. The primary purpose of a pillow is to keep your neck aligned with your spine while you’re sleeping. An improper pillow that doesn’t provide enough support or is too thick can cause your neck to bend unnaturally, leading to discomfort and pain.
A pillow that is too flat can cause your neck to tilt because it doesn’t provide enough support. On the other hand, a pillow that is too thick can raise your head too far up. The ideal pillow should adapt to the contours of your neck and head for optimal support. Memory foam pillows can mold to the shape of your neck and offer consistent support. Cervical pillows or neck pillows have a curved design that supports the natural alignment of the neck.
The mattress also plays a role in neck pain. A mattress that is too soft or too worn out will cause your body to sag into the bed, leading to poor sleeping posture. An overly firm mattress that does not conform to your body’s shape can also cause discomfort.
A medium-firm mattress is often the best choice for avoiding neck pain. It offers a good balance between support and comfort. Specialty mattresses like memory foam or latex are designed to contour to the body’s shape and distribute weight evenly to reduce pressure points. Ensuring that your mattress and pillow are suitable for your particular needs can significantly reduce the chances of experiencing neck pain after sleeping.
Can physical exercises or stretches alleviate neck pain caused by sleeping wrong?
Absolutely! Physical exercises or stretches can provide significant relief from neck pain caused by sleeping wrong. Here are a few recommendations:
**Neck Tilt**: Tilt your head forwards, so the chin touches the chest. Hold this position for 5 seconds and then slowly return to the neutral position.
**Side Neck Tilt**: Tilt your head towards one shoulder, leading with the ear. Hold for 5 seconds and return to the neutral position. Repeat on the other side.
**Neck Turn**: Look straight ahead and then turn your head to one side, keeping your chin at the same level. Do this for 5 seconds and then slowly return to the center. Repeat on the other side.
**Neck Stretch**: Stand tall and push your chin forward without moving your body. You should feel a stretch in the throat. Hold this for 5 seconds and repeat it in a normal position, then push it backward.
**Rolling Shoulders**: Roll your shoulders backwards and down 10 times, then roll them forward.
These exercises should not cause pain; if they do, stop immediately. It’s crucial to perform them slowly, without rushing, using smooth movements. Regular performance of these exercises can aid in reducing neck pain and preventing it in the future.
Are there any specific medical conditions that might cause neck pain after sleeping?
Indeed, certain medical conditions can cause neck pain that becomes evident or worsens after sleeping. The most common are:
**Osteoarthritis**: This degenerative joint disease can cause neck pain upon waking because it involves the breakdown of joint cartilage, leading to pain and stiffness.
**Spinal Stenosis**: This condition, typically caused by wear-and-tear, involves the narrowing of the spinal canal, which can compress nerve roots and result in stiff neck upon waking.
**Cervical Disc Degenerative Disease**: This condition involves the degeneration of the intervertebral disc, which could lead to neck pain, especially after staying in one position for too long, such as during sleep.
**Cervical Spondylosis**: This is a general term for age-related wear and tear affecting the spinal disks in your neck, which can trigger pain upon waking.
**Fibromyalgia**: This condition involves widespread musculoskeletal pain, fatigue, sleep, memory and mood issues. People with fibromyalgia can wake up with body aches and stiffness.
**Rheumatoid Arthritis**: An autoimmune disease that causes inflammation in joints, it can cause neck pain, especially after periods of inactivity like sleep.
**Cervical Radiculopathy**: Commonly known as a pinched nerve, this is caused by nerve compression in the neck, which can cause pain upon waking.
If you suspect that your neck pain after sleeping is due to an underlying condition, it’s important to consult a healthcare provider for accurate diagnosis and treatment.
Can physiotherapy care help with neck pain after sleeping?
Physiotherapy care can be very useful in managing neck pain from sleeping. Physiotherapists specialize in treating musculoskeletal conditions and can provide expert care for your neck pain.
Spinal manipulation: This can help improve spinal function and alleviate the cause of neck pain. These adjustments aim to restore the normal movement and position of the vertebrae in the neck.
Pelvic balancing: If the pelvis is uneven, it can cause postural changes in the neck, leading to discomfort. Pelvic balancing involves the physiotherapist addressing any imbalances in the pelvis to improve alignment and posture.
Ergonomic and lifestyle advice: A physiotherapist can provide advice on posture, ergonomics (work postures), exercises, and relaxation techniques. These tips can help relieve recurring joint irritation and tension in the muscles of the neck and upper back.
Soft tissue therapy: This involves the application of pressure to trigger points (tight spots in the muscle) in the neck and shoulders to relieve pain.
In conclusion, neck pain from sleeping is a significant issue impacting many people’s health and quality of life. Understanding its causes, symptoms, prevention methods, and treatment options can help us manage this issue more effectively and achieve a restful night’s sleep
Are you struggling with neck pain from sleeping?
Why Is It Hard To Stand Up After Squatting?
Why Squat Anyway?
As you get older or are more sedentary after working from home throughout the pandemic, it may seem more difficult to stand up straight after squatting. So what?” you might ask. “What’s the big deal?”
Actually, it IS a big deal, because the movement required to squat is also the movement required to get up from a chair or to bend down to retrieve something from a lower shelf. It’s a movement you’ll want to do throughout your life. In fact, here’s how squats can benefit your body:
- Overall strength. Each time you squat you get stronger and it makes the movement easier. You’re building a strong foundation for functional movement.
- Strong legs. When you squat, your legs get a workout, building strength and toning the muscles. Your glutes, quadriceps and hamstrings thank you.
- Core competence. Squats force you to stabilize your core, an area that is essential to balance and to almost any movement you make. This means the entire torso, including the abdominal muscles, the obliques and the lower back.
- Boosting your bones. As you build strength, you also build lean muscle mass, which supports your bones.
- Pregnancy preparation. While you’re strengthening your core with squats, you’re also strengthening your pelvic floor which makes delivery easier. For the aging population, it’s also beneficial to controlling urine leakage
- Jauntier jumps. If you’re a fan of pick-up basketball, you’ll find that strengthening your legs will add more height to your jumps.
- Power production. Squats can help you produce explosive power, important in jumping and sprinting.
- Injury prevention. Many injuries are associated with the body’s imbalances and weaknesses. Squats improve hip and knee stability, which can remedy numerous imbalances. It also takes some of the load off your knees and ankles, aiding ankle stability.
What Muscles Do You Use to Stand Up From a Squat?
Although you may not realize it, squats are a full body exercise. It may seem obvious that your abdominal muscles (core) are involved in helping you bend down and return to a stand, along with your glutes (buttocks), quadriceps (front of thigh), hamstrings (back of thigh) and calf muscles. However, numerous other muscles are involved in stabilizing other body parts as your rise, such as your feet, ankles, pelvis, hips and upper body.
Why Do I Struggle to Get Up From the Floor?
Sure, it’s easy to lower your body down to the floor. Getting back up again? That’s another challenge altogether. It’s a common problem, but one that isn’t healthy. It’s an indicator that you have issues with flexibility and/or mobility. Here are some of the possible reasons:
- Stiff joints. Lack of physical activity or immobility may make your joints stiff. Sitting at a desk all day certainly is a contributing factor. This means working on your mobility.
- Core crisis. If you feel off balance when you finally do get off the floor, it’s likely due to weak abdominal muscles, the core muscles that help stabilize your body.
- Weak muscles. If your legs feel weak and you wobble as you come to a stand, it may indicate a lack of overall strength.
- Nasty knees. If your knees are weak, you may feel as if they are unable to bear your weight.
What Muscles Do I Need to Strengthen to Get Up off the Floor?
If you’re looking to build enough strength and mobility to be able to get off the floor or out of a squatting position easily, your goal should be to do squats without toppling over or finding your knees locked. Your first port of call should be your registered physiotherapist, someone who is trained to identify weaknesses or imbalances in the muscles and joints and help people to remedy them.
Testing Your Mobility:
Meanwhile, here are a few tests you can do at home to see which joints may need some additional flexibility:
- Can you bend your ankle beyond 20 degrees? While standing, lift the ball of your foot off the floor.
- Can you flex your hip beyond 90 degrees? While standing, raise you knee toward your chest.
- Can you bend your knee beyond 90 degrees? While sitting, slide your heel back under your knee.
Once you’ve identified some weaknesses on your own, consult with your physiotherapist about the stretches you should do to begin improving your mobility. They will be able to assess your level of fitness and suggest exercises that are appropriate. As your strength and flexibility improve, they will adjust your exercises accordingly. Before you know it, you’ll be squatting with the best of them!
Is It Hard for You to Stand Up After Squatting?
What is Tendinitis?
If you’ve heard people talk about suffering from tennis elbow or runner’s knee, they’re referring to forms of tendinitis. Tendinitis is an inflammation or irritation of one of your tendons, the thick, fibrous cords that attach your muscles to your bones. Although it can impact any tendon in your body the tendons most usually affected are those in the shoulder, elbow, knee, wrist or heel.
Tendinitis Symptoms
If you have tendinitis, generally, you’ll feel pain in the area where the tendon attaches to the bone, as well as tenderness and mild swelling. The pain may interfere with performing basic daily tasks.
What Causes Tendinitis?
Tendinitis is generally a repetitive motion injury, occurring when the body repeats a specific motion over and over – especially if that motion is awkward. It may be job related, due to typing on computer all day or reaching overhead to store and retrieve boxes from shelves, and or it can be sports related, as with a baseball pitcher who uses his shoulder to hurl the ball regularly.
As you age, your tendons become less pliant and flexible, so you may be more prone to tendinitis. However, it can also result from poor technique in executing a motion or from a sudden impact.
Physiotherapy for Tendinitis
If you experience symptoms of tendinitis in any of your joints, it’s time to talk to a registered physiotherapist. They are trained to assess and treat such injuries and will help you recover so that you can return to your usual activities safely and pain-free. However, be prepared to take things slowly, because the body doesn’t deliver large amounts of blood to the tendons in comparison to your muscles, so healing completely may take time.
Your physiotherapist will customize the treatment to your injury. They will show you how to reduce stress on the affected area by correcting your body mechanics and posture. They will manipulate the area manually, doing some gentle stretches and joint movements to improve mobility in the area. They may also use other methods to promote healing, such as trigger point dry needling, an acupuncture technique that can affect the way the brain and muscles communicate, allowing your system to return to a more normal movement pattern. Your physiotherapist will also prescribe exercises to improve your body’s healing without overloading the affected area.
Get Relief for Tendinitis
If you are in pain and wonder if tendinitis is the cause, don’t hesitate to consult with a registered physiotherapist. Left untreated, tendinitis can lead to a ruptured tendon and possible surgery.
Suffering from a Repetitive Motion Injury?
Understanding Active Release Technique
If you’re suffering from a sports injury, an overuse impairment or chronic pain, it can be helpful to consider therapy in the form of Active Release Technique (ART) to alleviate the pain and restore your range of motion.
How Does Active Release Therapy Work?
Active Release Technique is a method of non-invasive manual therapy that combines manipulation and movement to correct soft tissue injuries that restrict movement and cause pain.
Tissues are subject to negative changes from trauma. ART is employed to break down scar tissue and adhesions in your body, promoting blood flow and healing to affected areas. Scar tissue can be binding, causing your muscles and joints to feel painful and stiff.
ART treats issues with muscles; tendons, which connect muscle to bone; ligaments, which connect bone to bone; fascia, the fibrous tissue that supports and protects and supports muscles and organs; and nerves.
The History of Active Release Technique
Active Release Technique is a treatment method that was developed in the 1980s by a chiropractic doctor, Michael Leahy, who was frustrated by the slow pace and inefficiency of traditional means for healing soft tissues, especially for Olympic athletes who needed quick results in order to return to competition. In 2001, he was granted a patent for his soft tissue treatment system. Physiotherapists, chiropractors and others must receive training and certification to become ART practitioners.
ART for Soft Tissue Injuries
ART has proven to be successful for a variety of soft tissue injuries where scar tissue has accumulated. Some of the signs that you may have a buildup of scar tissue include increased pain when exercising; reduced flexibility and limited range of motion; inflamed joints; decreased strength; and tingling, numbness or weakness.
Scar tissue is part of the body’s normal response to healing. It’s a dense, fibrous material that forms as a result of injury to connect and bind injured tissue. Unfortunately, it isn’t as flexible as normal tissue. As a result, muscles can weaken and shorten and nerves can become entrapped, leading to pain and dysfunction. ART can relieve pain and restore function to the affected areas.
Common Conditions Treated by ART
ART practitioners use this technique to address acute injuries, such as tears and sprains; chronic trauma, such as ongoing lower back pain; overuse trauma, such as repetitive strain injuries; and post-operative cases. It is ideal for people with overworked muscles. Some of the common conditions treated by ART include neck pain, runner’s knee, golf or tennis elbow, tendinitis, frozen shoulder, sciatica and carpal tunnel syndrome.
Diagnosis and Treatment
An ART practitioner will use his/her hands to discover anomalies in tissue texture, tension and movement to pinpoint the cause of the problem. Once the problem is identified, your physiotherapist or other ART practitioners will employ ART treatment protocols to restore the tissue’s proper function and relieve pain. This is done by working with the tissue while it is in an active position, applying hands-on tension.
The patient may be required to move the affected area/body part to achieve full release. The experience is reminiscent of massage, combined with movement and stretching. However, your physiotherapist will focus on targeted contact points, rather than using broad strokes.
ART can be intense because it involves precise pressure. Although it may be uncomfortable, it generally yields results in five sessions or fewer.
Post-Treatment Exercises
Once a patient is treated with ART and the restrictive adhesions have been broken up, it’s important to prevent the symptoms from recurring. The patient needs to take an active role in prevention by doing exercises that address four fundamental areas:
- Strength: Strengthening exercises are most valuable once adhesions and scar tissue have been treated, because any attempt to strengthen shortened and contracted muscles may lead to further restriction.
- Flexibility: Flexibility refers to allowing for full range of motion, and it is specific to a particular joint. A patient may have full range of motion in the shoulders, but be constricted at the knees. Stretching done prior to ART won’t actually reach the affected area and may lead to further biomechanical imbalances. Stretching once ART is complete is essential.
- Balance and Proprioception: Proprioception exercises are designed to restore a patient’s kinesthetic awareness, allowing the body to react appropriately to external forces. They form the foundation for the strength, endurance and agility needed for complete rehabilitation.
- Cardiovascular: Aerobic exercise increases blood flow and oxygen delivery to soft tissues. Poor circulation and lack of oxygen accelerate repetitive strain injuries.
Why Active Release Technique?
ART is unique among treatment modalities because it involves more than 500 specific manual therapy techniques that target restrictions in various soft tissues. There are no known side effects and most conditions are restored in five sessions or fewer.
Suffering from a sports injury, an overuse impairment or chronic pain?
What to Do for a Stiff Knee
It’s no fun to have a stiff knee or to feel aches and pains in your knee joints. Knees are so central to our ability to move easily, that any hiccup in their smooth operation can be very frustrating. Luckily, there is help available in the form of medication, physiotherapy and – as a last resort – surgery.
Knee pain can be caused by arthritis, repetitive trauma, a strain or another injury. The knee is a hinge joint and its workings are complex. It is the spot where the shin bone (tibia) and the thigh bone (femur) join, supported by four ligaments, tendons and cartilage that acts as a shock absorber (meniscus). The kneecap (patella) protects the joint. An injury to any of these components or more than one is likely to produce stiffness and pain in the knee, as will osteoarthritis, or chronic inflammation of the joint.
If you suddenly develop knee pain, the first steps should be the RICE treatment regimen: Rest your knee, Ice it to prevent or lessen swelling, Compress (bandage) it for support and Elevate it to send healing blood flow to the area.
Next, it’s wise to have your physician or trained physiotherapist examine you, diagnose the problem and suggest the appropriate long-term solution. If some components of your knee joint aren’t working properly and you ignore the aches and pains, other parts of the knee will generally compensate and the stress that results can lead to chronic issues.
What Causes Stiffness in the Knee?
The root of your knee problems will depend on where you are experiencing pain or stiffness. Pain at the front of the knee may be caused by problems with the position and tracking of your kneecap — a condition known as patellofemoral stress syndrome (PFSS) – that may involve swelling of the kneecap and the tendon connecting the kneecap and shin.
Pain on the outside of the knee may indicate an injury to the medial meniscus or medial collateral ligament, often damaged during exercises that involve twisting. Pain to the outside of the knee can have many causes, including injury to the hamstring tendon or a ligament. One common culprit is stress to the iliotibial band, a thick band of muscle running from the outside of the hip to the front of the knee, where it can rub and abnormally.
There is also pain at the back of the knee, which is rarer, but could be caused by a cyst or by an injury to the hamstring, which attaches there.
Assessment
Your trained physiotherapist will generally assess your injury using a variety of techniques that may include an analysis of your gait to see how you walk; measuring range of motion to see what capabilities your knee has; measuring your knee’s strength to determine if you have a muscular imbalance; and palpation, hands-on assessment to check for swelling, abnormalities and pain.
What Is the Best Exercise for Stiff Knees?
Exercises targeted to your specific knee problem will be prescribed as the main treatment. Often, this involves strengthening the knee itself, as well as the surrounding supports that can help take pressure off the knee itself. These exercises will generally include balance exercises, lower extremity stretches, straight leg raises and hip strengthening, since your hip muscles help control your knee position.
In addition, your trained physiotherapist may employ techniques such as ultrasound, soft tissue massage, acupuncture, electric stimulation and kinesiology taping.
If your pain is due to arthritis, movement is essential to keep your joints lubricated. There is currently no cure for arthritis other than knee replacement surgery, but the symptoms can be managed and controlled.
How to Prevent Knee Stiffness and Pain
Lifestyle modifications can help you keep your knees healthy and strong. You’ll want to maintain a healthy weight, because excess kilos put pressure on your knees. Keeping your hamstrings and quadriceps strong will assist your knees, because these muscles provide support to the knee joints. If you participate in sports, be sure your technique is solid so you aren’t putting unnecessary pressure on the knee joints.
In addition, be sure to warm up sufficiently before you exercise. Stretch your legs before and after you participate in a sport or athletic endeavour; do so slowly.
Remember, knee pain is a signal your body is sending to let you know that something is wrong. Don’t exacerbate the injury by ignoring signals. When you feel pain, employ the RICE method and make an appointment with your physiotherapy professional.
Knees Stiff or Sore?
Working from Home Ergonomics: A Guide to Preventing Injuries
As the days of the pandemic turned into months, it became obvious to Canadians working from home that their makeshift office settings were leading to unexpected consequences – new aches and pains in various parts of the body and possible musculoskeletal injuries.
The New Year is the perfect time to take a look at how to prevent injury from your home work setup and get into new, healthier habits. Where and how you work are important to your health. Meanwhile, your physiotherapist can assist you with the appropriate exercises and recovery plan if you’ve already fallen victim to home workplace injuries, such as back strain or carpal tunnel syndrome.
Ergonomics at Home: How to Set Up Your Office
No matter how crowded your quarters, sitting on the couch or bed with your laptop just isn’t wise – you’ll soon be feeling back pain, neck or wrist strain. Even though you may not be able to achieve an ideal setup at home, do what you can to help your body stay healthy. Here are some tips for setting up your workspace in a more ergonomic fashion:
Lighting.
Make sure the lighting in your workspace is adequate; working in rooms that are too dark or too brightly lit can lead to eyestrain and headaches. You also want to avoid glare, so reduce or eliminate it with window shades, diffusers on overhead lights and anti-glare filters for your computer screens.
Seating.
A chair with proper lumbar support can protect the lower back from injury and keep your spine aligned. You can use a rolled-up towel or a pillow as a support. If possible, use a chair that can be adjusted to your height. Sit with your feet flat on the floor and keep your knees, elbows and hips at about 90 degrees. Your wrists should be aligned with your elbows and your eyes should be in line with the top of your screen. A thick book or a ream of paper is useful in raising your monitor or laptop to align properly and the rolled towel or a pillow also work magic in aligning your wrists and elbows.
Computer Setup.
Your computer monitor should be an arm’s length away to prevent you from bending your neck forward and straining it or causing eye strain if it is too close. Your keyboard and mouse should be placed in a way that allows your wrists to be straight so you avoid carpal tunnel syndrome. Keep your cords taped down or tucked away so you avoid tripping.
Desk Design.
Further ensure that your workspace is ergonomic by organizing your desk accordingly. Items you use frequently, such as your mouse, your keyboard or a pen, should be within a forearm’s reach, while things you use less frequently, such as scissors, tape or sticky notes, could be placed within an arm’s length. Equipment that isn’t used often, such as a printer or a scanner, can be situated further away.
Working From Home: Injury Prevention Strategies
Setting up your home office is only half the battle in staying healthy while working from home. Self-scrutiny and maintenance are also important. Take note of these hints:
Monitor Your Posture.
Keep an eye your alignment while you’re working. Be sure that the there is no pressure under your thighs, that the small of your back is supported and your shoulders are relaxed (not slumped and not elevated).
Take Frequent Breaks.
Sitting for long periods of time can be harmful to your body, so take lots of mini-breaks to allow your muscles and joints to move and recover. Do some stretching or take a short walk. You can set a timer or your watch or download an app to remind you to stop your current task and get up from your desk. Don’t skimp on breaks; your body will thank you later. Yoga is also a wonderful way to stretch overused joints and muscles.
Pay Attention to Discomfort.
You are not being a whiner if you have concerns about new aches and pains; your body is trying to tell you something. Adjustments to your work station may right the ship, but, if not, contact your physiotherapist for an evaluation and some preventive or rehabilitation exercises. Working through your pain may simply make the problem worse and harder to correct.
Life is all about change, and the better you adapt to the changes to your work environment, the happier your body will be. However, if you are experiencing discomfort, don’t hesitate to get in touch with your physiotherapist to put you back on course.
Is Working From Home Causing You Pain?
The Benefits of Physical Therapy Throughout Your Life
Many people associate physical therapy with injury. You see your physical therapist when you’ve sprained an ankle playing tennis or injured a knee while running and are eager to heal properly so you can get right back at it.
It’s time to look at physical therapy in a different light: as a lifelong helping hand that works to keep you pain free and healthier. Remember, it’s not a choice between seeing your doctor or your physical therapist; physical therapists work with other health-care professionals to ensure you get the best possible treatment for your needs.
The Benefits of Physical Therapy
Let’s take a look at many of the benefits you can derive from taking advantage of physical therapy on an ongoing basis.
Managing Pain
If you have chronic pain, you know that it can be debilitating – but it needn’t be. Physical therapy techniques and therapeutic exercise will help you mobilize your soft tissue and joints and restore function to your muscles. Your pain will be reduced or eliminated, and if you continue your exercises, you’ll be able to prevent pain from returning or climbing to previous levels.
Avoiding Surgery
Physical therapy can be the first line of defence when it comes to surgery prevention. Why jump immediately to potentially costly and invasive procedures, when physical therapy can help you banish pain, promote healing and offer better all-around health, which may help the injured tissue to heal and allow for mobility? Surgery is unavoidable in some cases, but not all, so consider your options.
Assisting with Age-related Issues
As we age, we often develop age-related health problems, such as arthritis, osteoporosis and joint pain. Physical therapy is a good starting point in managing those issues, because it doesn’t require joint replacement, and it is useful in managing pain.
Aiding Recovery
If you injure yourself or do need surgery for a health issue, physical therapy can help speed your recovery. Rather than ignoring your pain or trying to Google your injury and heal yourself, why not talk to a professional? Physical therapy treatment helps improve mobility and balance and will help you get back on your feet more quickly. After surgery, it helps restore joint function, builds up strength in your muscles, assists you in returning to the activities of daily living, reduces pain, eases swelling and improves circulation, which is important in preventing blood clots.
Boosting Your Immune System
Regular exercise improves the body’s immune system and physical therapy is one way of ensuring you’re getting it. For some people, physical therapy is the only exercise they do all day. Exercise leads to good health and a healthy immune system, so don’t neglect it.
Trying New Activities
Often, after a patient has physical therapy and experiences the benefits that stretching and resistance can have for their bodies, they are emboldened to try a new type of exercise or physical activity. They take up a new sport, go to the gym or start a regular exercise regimen at home. Yoga or elliptical trainers, anyone?
Avoiding Dependence on Medications
If you’re injured or recovering from surgery, you may be taking medications to blunt the resulting pain. You may even have a prescription for opioids, which are effective in dulling pain, but are highly addictive. During COVID-19, Canada’s opioid crisis hasn’t received the attention it did previously, but the problem hasn’t disappeared.
Reducing Fall Risk
As we age and become frailer, we’re often at greater risk for falls. Physical therapists can work with us to increase strength and endurance and improve balance to reduce the possibility that we’ll fall and end up with a debilitating broken hip.
These are only some of the ways physical therapy can benefit you throughout your life. Physical therapists work with you to determine your physical goals and help you achieve them. Even better, especially during the pandemic, they can work with you virtually to ensure you get the treatment you need.
Are You Ready To Give Physiotherapy a Try?
New Mother Aches and Pains: How Physiotherapy Can Help
Pregnancy is a wonderful, joyful time for many expectant mothers, but it can be accompanied by a slew of physical discomforts: heartburn, headaches, morning sickness, fatigue and insomnia to name a few.
Pregnancy also strains the back, neck and hips of expectant mothers by shifting their centre of gravity. New moms may think that once their bundle of joy has arrived, the various aches and pains will disappear, too. However, often that’s not the case.
New moms can be prone to various repetitive strain injuries as a result of carrying and nursing a new baby. Here are some of the most common new mother aches and pains and what you can do about them.
New Mom Backaches
New moms can develop a sore back from bending to pick up their baby, leaning over a crib to calm and settle their baby and leaning into a car to place and secure an infant car seat. Over time, this can develop into a repetitive strain injury.
Preventing Postpartum Backaches and Pain
You can prevent postpartum back strain by:
- Checking and correcting your posture when performing tasks that require using your back, such as lifting and carrying.
- Make sure your feet are flat on the floor and shoulder width apart when lifting.
- When changing direction, move your feet with your body instead of twisting your spine so that you keep your back straight and in line with your hips and knees.
- Lift by bending your knees and hips instead of your back.
- Do regular exercises, such as Pilates, to strengthen your core and abdominal muscles to reduce the pressure on your back.
Neck Pain From Breastfeeding
Nursing mothers experience neck pain most often because of poor posture during breastfeeding. They assume awkward positions of leaning forward and looking down while sitting. When they do this for half an hour every few hours, they put a lot of strain on the neck and surrounding muscles in the shoulders and back. It can even give new moms headaches.
Preventing Nursing Mother’s Neck
Prevent nursing mother’s neck by:
- Setting up a feeding station in a comfortable chair.
- Use a pillow to support the arm holding the baby and another pillow behind your low back.
- Avoid slouching.
- Do some gentle neck stretches after each feeding.
Mother’s Wrist and Mommy’s Thumb
An empty infant car seat has a mass of four to five kilograms. Carrying so much weight strains the wrists and elbows, and, over time, can cause repetitive strain injuries.
A new mom can also develop Mother’s wrist or Mommy’s thumb by overflexing the wrist and thumb from carrying the baby. Not only does carrying the baby eventually become painful, but so do other activities, such as turning door knobs and opening jars.
Preventing Lower Arm Strains
To prevent straining the lower arms:
- Switch sides regularly when carrying your baby. Alternatively, use a front or back carrier to distribute your baby’s weight evenly on your back and shoulders.
- Take regular breaks to stretch your neck, back, arms and wrists.
- To lift an infant car seat out of the car, place both hands on the handle and keep your elbows bent.
- Carry an infant car seat in front of you with both arms to distribute its weight.
- If necessary, wear a splint on your wrist and thumb to alleviate pain.
Pelvic Pain and/or Incontinence
Women usually carry a baby on the hip that’s opposite their dominant hand. When you carry your baby on one side, your pelvis can shift, which can cause pelvic and hip pain and sometimes lead to an uneven gait. In addition, some new moms experience incontinence due to pelvic floor weakness caused by pregnancy and delivery.
Preventing Pelvic Pain and/or Incontinence
- To prevent pelvic pain, switch sides regularly when you carry your baby.
- To treat incontinence, see a pelvic floor physiotherapist to assess incontinence, as well as pelvic pain.
How Physiotherapy Can Help New Moms
In addition to these helpful tips, physiotherapists can recommend exercises for treating and preventing all these repetitive strain injuries that often are just part and parcel of being a new mom. A physiotherapist can provide education on new mother aches and pains, as well as a referral to a pelvic floor specialist.
New motherhood is an amazing experience. Make sure that you’re also looking after yourself so you can give your new baby the best possible care.
Experiencing New Mother Aches and Pains?
The Scoop on Overuse Injuries
As research has shown, exercise is extremely beneficial for both our body and our mind. It keeps the body strong and healthy so it can fight off illness successfully and it elevates our mood, keeping depression at bay.
Unfortunately, we can’t always exercise as much as we might like, due to injury. We’re all familiar with major injuries — also called acute injuries – such as broken bones or sprained ankles that result from a single blow or fall. Most of us are less familiar with overuse injuries, injuries that result from frequent, repeated use of muscles, joints, tendons, ligaments and bones.
Overuse Injuries
Overuse injuries, also categorized as microtraumas, result over time from repeated action. They include minor sprains to ligaments, muscle strains, overstretched tendons and small tears in the connective tissues and fibres of our muscles.
Exercise generally strengthens, muscles, tendons, ligaments and bones by breaking down old tissue and allowing new tissue to grow. However, if tissue breaks down faster than it can be rebuilt, overuse injuries occur. When we engage in a physical activity too intensely or for too long (such as typing), or we do too much before our body is ready, our body’s structures don’t have enough time to rebuild before they are used again.
Improper technique while exercising can also put stress on the body and lead to overuse injuries, as can favouring a particular body part, such as an uninjured ankle when the other is sprained. Overuse injuries can also result from changing equipment, such as the shoes you wear during exercise.
The causes of overuse injuries can be categorized as poor core stability, muscle imbalance, incorrect equipment, faulty technique, biomechanical issues or lack of necessary strength or endurance.
Symptoms
You are likely to have an overuse injury if:
- You feel pain immediately or within 12 hours of exercising;
- You feel pain while exercising, but it doesn’t prevent movement and disappears afterward;
- You feel pain during exercise and it prevents certain movements, but disappears afterward; or
- Chronic pain that prevents you from moving and doesn’t improve.
Overuse injuries often show signs of inflammation, such as minor swelling, warmth to the touch, impaired function and/or redness.
How Are Overuse Injuries Treated?
In treating an overuse injury, the first step is to remove the cause. Don’t use the injured body part until it has time to heal and the pain disappears. You can ice the affected area and use over-the-counter anti-inflammatory medications to reduce swelling and relieve symptoms.
You’ll also want to consult a physiotherapist for a proper course of treatment. They will prescribe exercises that help heal and strengthen the injury and its supporting structures. As you heal, they will adjust the type, frequency and intensity of these exercises.
Once you are ready to use the injured part regularly, you’ll need to warm up properly before each exercise session. Your physiotherapist can also advise you on a proper warmup routine. You may also want to consider varying your workouts or activities.
How to Avoid Overuse Injuries
It’s worthwhile taking precautions to prevent overuse injuries. Some of the strategies you can use to stay fit and healthy include:
- Listening to your body and resting when you feel soreness or pain;
- Warming up properly before each exercise session;
- Gradually increase the intensity, duration and distance for your activity;
- Obtaining instruction from a trainer on how to use equipment correctly;
- Planning on two rest days each week so your tissues have time to rebuild;
- Using the proper equipment; for work-related injuries, being sure that your work station is set up ergonomically.
Your body is, as they say, your temple; worship it and it will serve you well in return.
Overuse Injury Causing You Trouble?
Preventing Back Pain for Flight Crews and Travellers
Air travel is a fact of life for many of us, whether because it’s our livelihood, our work demands it or we want to explore places that are most easily accessed by flying. There were 600 licensed air carriers in Canada in 2018 and just over 159 million passengers boarded and unloaded in Canada last year; 34.7 million of them were Canadians. In addition, for each of the flights that took off or landed in Canada, there were air crews to add to the totals.
Unfortunately, flights longer than an hour aren’t always the most comfortable for our backs and may cause or aggravate injuries. Back pain, as many of us know from personal experience, is no joke, and it is also fairly common. Statistics Canada notes that four out of five Canadians will experience at least one incidence of back pain during their lives, with the pain most likely to occur in those between the ages of 30 and 50. Back pain can impede mobility and affect quality of life, so it’s something we’d all like to forego.
Causes of Back Pain While Flying
Whether we’re flying for work or pleasure, knowing how to prevent and address the concomitant back pain is essential. For passengers, threats to our backs include long periods of sitting or standing, sleeping in an unnatural position, travel stress, lifting heavy objects, such as suitcases, and twisting the body while you’re lifting something.
For air crews, the list includes heavy lifting, reaching and lifting, twisting while lifting or holding a heavy load, lifting or carrying objects with odd shapes, sitting or standing for prolonged periods in one position, working in awkward positions, slipping on a wet floor and, perhaps, poor sleeping positions.
Preparing for the Flight
If you’re planning a trip, you can take some steps in advance to ensure that you won’t incur a back injury, or even a twinge:
- Get a Doctor’s Note. Your physician can provide you with a letter requesting certain accommodations that will make travel smoother. These can include the ability to walk around during the flight, permission to lie down on the floor and rest, additional pillows and blankets and a possible upgrade to business class.
- Contact the Airline. If you let your carrier know about any back issues, you can also request a wheelchair to take you from security to boarding, assistance with lifting and carrying luggage and help in boarding.
- Pack Lightly. The fuller your bags, the heavier they are to lift and carry. Check your bags, if possible, so you have no need to hoist them into an overhead bin. If you do have a carry-on bag, ask one of the flight attendants to assist you in lifting it.
- Adjust Your Schedule. If you have a choice, fly at a less-busy time of day so you’ll have more room to move about the aircraft and an easier time getting to the aisle, stand or stretch.
- Prevent Inflammation. Pack your carry-on bag with ibuprofen or any other relevant medication that prevents back pain and reduces inflammation, especially if it’s an ongoing problem.
- Keep Exercising. Maintain your exercise routine in the days leading up to a trip. Sitting in cramped quarters if you haven’t been exercising could cause muscles to spasm. Exercise keeps your muscles flexible.
Back Pain Prevention In Flight
No one is eager for a back injury, especially with the chance that it could become chronic. Here are some tips for coping with the standard discomforts as a passenger:
- Keep Moving. Unless you’re one of those travellers who can sleep through a flight, try to book an aisle seat to make it easier to get up and walk around or stand. Doing so will help alleviate any pain and stiffness you feel from sitting in one position.
- Recline Your Seat. Yes, it may crowd the person behind you, but it relieves the pressure on your discs caused by the standard sitting position. You will be supporting some of your weight with the backrest, rather than your spine.
- Use a Back Support. Lumbar rolls and back braces can provide you with additional spinal support while flying. Use a roll (or a rolled-up sweater) that supports your lower back without pushing it away from the seat.
- Stay Hydrated. Drink water and more water for a few days in advance of travel and during travel. Cabins are dry, which can exacerbate back problems. The gel in the inner discs of the spine is also susceptible to dehydration, so drinking water is a good preventive measure against tears and bulges.
Preventive Measure for Crew Members
Airline attendants are subject to different stresses and strains that can cause back injuries. These tips can help them to keep back injuries at bay:
- Stay Fit. You’ll need good fitness to endure long flights with all of the standing, bending, lifting and reaching your job requires. A strong core, especially, is important for preventing back injury and pain. Cardiovascular fitness is also valuable.
- Stand Properly. When you’re on your feet, keep your head in line with your shoulders and be sure your shoulders are in line with your pelvis. Draw your buttocks and abdomen in gently – a protruding abdomen puts undue pressure on your spine. Place your feet a shoulder-width apart to distribute your weight evenly. Don’t tense up – it may actually contribute to back pain.
- Lift With Care. If you need to lift heavy loads, do so from hip level or lower. Bend at the knees, not from the waist, to prevent injury to your back. Your body isn’t designed to twist like a Gumby; avoid doing so when you lift. Move your entire body when you turn, rather than shifting only your upper body. Keep the load close to your centre of gravity – at your chest, rather than down near your hips.
- Don’t Overreach. When you reach with one hand, be sure to find a stable anchoring point with the other.If you use your feet alone to balance while the trunk is tight and twisting, you can pull muscles in your lower back.
- Watch Those Bends and Turns. If you need to bend, do so from the waist and don’t turn at the same time. Turn the entire body, rather than turning from the waist.
If you have concerns about back pain, either before or after your flight, your physiotherapist can be invaluable helping you address your concerns.
Is air travel causing you back pain?
Warehouse Work Causing Back Pain
With the rise of Internet shopping, the warehouse – and the warehouse worker – has become a more visible part of the supply chain. When bricks-and-mortar stores were the usual destination for purchasing goods, it is unlikely that consumers gave much thought to where their goods had been stored before being displayed by a retailer. Today, however, as more and more people order goods online – 87 per cent of Canadians made at least one online purchase last year, according to the Canadian Registration Internet Authority — warehouses figure prominently in the packaging and delivery of those items and get more attention.
Warehouses and Back Injuries
Along with warehouse work come back injuries. Canada’s Workplace Safety and Insurance Board (WSIB), the organization that handles workplace injury claims, reported in 2017 that the lower back was the body part that resulted in the largest amount of lost-work time, accounting for 17 per cent of all claims.
Overexertion was the leading cause of injury for materials handlers, especially those ages 20-24, with the lower back the area most affected, usually by strains and sprains. However, warehouse workers are also subject to other injuries, such as pulled muscles and pinched nerves. It’s no real surprise, considering all of the bending, lifting, twisting and quick shifts in motion that are part of the job.
For example, bending down to reach low shelves and lifting heavy items up can be injurious. Warehouse employees also need to be constantly on the lookout for fallen objects, spills and moving vehicles so they can remain safely on their feet. In addition, vibrations from forklifts used to move boxes and crates cause wear and tear on the body.
Even sitting to do paperwork to document your work or standing around waiting for your next task can be tough on your back. Most of us don’t use proper posture when we’re in our chairs or on our feet and our backs suffer for it.
Prevention is Essential
That’s the bad news. The good news is there are things you can do to prevent back injuries. Your physiotherapist can develop a course of stretching and exercise designed to strengthen your back muscles and ensure you are prepared for the repetitive motions your job requires. It’s important to use the proper technique, because even minor injuries and a poor physical approach to your tasks can lead to recurrent or chronic back pain.
There are also other keys to maintaining a healthy back. Take note of these tips and you’ll have the best chance of keeping your back in good shape:
- Stretch. Stretching loosens tight muscles and improves flexibility while preparing your body for periods of exertion, along with sitting and standing. Don’t simply stretch prior to the start of your workday; take regular breaks to do a few simple stretches. They’ll help reinvigorate your back muscles and banish those kinks that appear during the course of the day.
- Lift and Carry With Care. If you need to lift heavy loads, do so from hip level or lower. Keep the load close to your centre of gravity – at your chest, rather than down near your hips. Bend at the knees, not from the waist, to prevent injury to your back. Avoid twisting when you lift; your body isn’t a corkscrew! Move your entire body when you turn, rather than shifting only your upper body.
- Take Care of Your Tootsies. Your feet are important supports, especially in warehouse work, which requires you to stand much of the day. When your feet are uncomfortable, it places more stress on your back, so be sure you wear supportive footwear. Custom orthotics work well for people who spend most of the day upright. You don’t want to end your shift aching and in pain, so treat your toes well. You’ll feel the difference at day’s end.
- Stand Properly. When you’re on your feet, keep your head in line with your shoulders and be sure your shoulders are in line with your pelvis. Draw your buttocks and abdomen in gently. Place your feet a shoulder-width apart to distribute your weight evenly. Don’t tense up – it may actually contribute to back pain.
- Sit Correctly. If you spend part of your time doing paperwork, be as conscious of your seated posture as your upright stance. Place your feet firmly on the ground and your buttocks in the space between back in the chair and the seat. Align your knees with your hips. Make sure your chair allows you to rest your arms at elbow height. Keep your computer screen at eye level.
Finally:
- Know Your Limits: Your employers don’t expect you to be Hercules, and you shouldn’t expect it of yourself. Excessive pride can lead to injury. If you need a hand in lifting something heavy, ask for it!
- Don’t Ignore Pain: Pain is your body’s way of telling you something is wrong. If you feel even a twinge, accept it as a signal that you need to make an adjustment, whether in your lifting technique, your standing posture or your job itself. Don’t hesitate to visit your physiotherapist for an assessment and some solutions.
Is warehouse work causing you back pain?
Why are my shoulders sore?
You’ve heard your friends describe someone by saying, “He carries the world on his shoulders.” It’s a saying that derives from Greek mythology and it refers to Atlas, the Titan god who held the sky aloft. When the Titans were defeated by Zeus, Atlas was condemned to carry the heavens on his shoulders and he is often pictured as a man bending forward, holding the Earth on his back. Now, who wouldn’t have sore shoulders from such a challenge?
While you don’t literally carry the world on your own shoulders, figuratively, you may feel as if you do. Life is full of stress and challenges and our shoulders absorb much of that tension. In addition, our shoulders are the joints with the greatest range of motion and are ripe for injury. Luckily, there are ways to ease your physical burden.
How do you relieve shoulder pain?
Naturally, some sources of shoulder pain require more serious remedies than others, but all are treatable. There is no need to suffer unduly. The appropriate treatment for your shoulder pain depends on:
- Severity of the injury;
- Location and type of injury;
- How long ago it occurred;
- Your own age and general health; and
- Your usual activities.
If your shoulder pain is the result of an acute injury such as an automobile accident or a blow to the shoulder, don’t delay in seeking a medical evaluation and suggestions for appropriate treatment. Fractures need to be stabilized quickly so they can set properly.
Rest for a day or two and regular applications of ice to control inflammation and keep the pain in check are generally appropriate for all shoulder injuries. You may also want to take a non-steroidal anti-inflammatory device (NSAID), such as ibuprofen, to reduce the pain.
Physiotherapy
Your physician will undoubtedly suggest a visit to the physiotherapist once the pain and swelling have subsided a bit. A physiotherapist will assess the injury, its causes and the associated pain and will create a course of treatment. You can expect questions about the source and severity of your shoulder pain, as well as the factors that aggravate it or relieve it.
Your physiotherapist will also test your range of motion and shoulder strength before determining which exercises and other treatments will be most beneficial. Remedies such as moist heat and acupuncture are among the options available to supplement exercises.

The anatomy of the shoulder
Your shoulder is a ball and socket joint that consists of three major bones: the upper arm bone (the humerus), the collarbone (the clavicle) and the shoulder blade (the scapula), bound together by tendons, ligaments and muscles. With so many moving parts, it’s no wonder that shoulders are easily injured. In addition, the joint overlaying the shoulder, the acromioclavicular joint, is also subject to injury.
What causes shoulder pain?
Shoulder pain can result from chronic ailments, such as osteoarthritis, or from an injury to the joint or its surrounding parts. Common causes of shoulder pain include:
- Arthritis
- Strains from overexertion
- Tendinitis from overuse
- Pinched nerves
- Dislocation
- Fractures to the collarbone or upper arm
- Joint instability
- Frozen shoulder
- Pulled muscles (sprains) or injuries to the ligaments (strains)
- Damage to one of the surrounding tendons (torn rotator cuff)
- Poor sitting posture (hunching over a computer all day, for example)
Some of these injuries are acute and caused by trauma to the area. You may fall and land on your arm in an awkward position; you may twist or bend your shoulder abnormally, perhaps pitching in a pickup baseball game; or you may absorb a direct blow to the shoulder, falling on the stairs, for example.
In other cases, the injuries may be the result of overuse and sneak up on you. Overuse injuries result when too much stress is placed on the joint, through repetition of a motion or by overdoing an activity. Your tennis serve may put repeated stress on your shoulder until, finally, injury results.
In addition, there are seemingly benign sources of shoulder pain, including poor posture and muscle tension.
Can stress cause your shoulder to hurt? Yes, stress can accumulate in the shoulders as easily as it does in other joints.
Overuse injury symptoms
Naturally, if your shoulder injury is due to trauma, such as a tackle during a football game or a fall down the stairs, you’ll be able to identify the cause immediately. However, if your injury is due to overuse, these symptoms may be signs that you need treatment:
- Limits to your range of motion;
- Loss of strength in your shoulder;
- Shoulder pain and stiffness;
- Difficulty in doing everyday tasks, such as bathing, driving a car, dressing and sleeping comfortably; and/or
- Problems with accomplishing tasks that require you to put one arm behind your back, such as zipping a dress.
How to prevent shoulder pain
Shoulder problems can usually be repaired without surgery. Nonetheless, why endure them at all when you can take some simple steps to prevent them:
- Stay in shape: Eat a healthy diet and exercise regularly.
- Warm up before exercise: Cold muscles are more susceptible to injury.
- Watch your posture: Sit and stand erect. Get up from your desk every hour to move around and stretch.
- Lift properly: Don’t strain to reach items you need. Step stools were created to help you.
No matter whether your shoulder injury is minor or major, it will heal with proper treatment. There’s no need to live like Atlas for the rest of your life!
Let's get you some relief for your shoulders!
What Causes Neck Pain?
At one time or another, you’ve undoubtedly muttered to yourself, “What a pain in the neck.” Of course, you’re generally referring to an annoyance, not to a literal ache in the real estate that connects your head to your shoulders. Nonetheless, there will come a time when your neck does ache and you’ll wonder why and what to do about it. Let’s demystify neck pain so you know how to react when it occurs.
Causes of Neck Pain
Neck pain refers to pain that occurs anywhere in the region starting at the base of the skull and ending at the shoulders. The neck comprises the bones and joints of your cervical spine, otherwise known as your neck vertebrae; the muscles and ligaments that keep the cervical spine together; and the discs separating your vertebrae and serving as shock absorbers.
It’s not unexpected that your neck muscles, ligaments and bones are subject to the same wear and tear as the rest of your body. Overuse, poor positioning or injury can take their toll, leading to stiffness, soreness or extreme pain.
Chronic conditions are one cause of neck pain. Damage to the discs in your neck over time can lead to a pinched nerve, causing pain in one side of the neck that may involve tingling, numbness and pain that radiates down to your hand, while osteoarthritis can cause pain due to joint breakdown.
In addition, poor positioning of your neck may also cause pain or stiffness, and there are numerous culprits for such behaviour. You may spend a lot of time hunched over your computer or your cellphone; you may sleep with your neck at an odd angle; or you may angle your neck unnaturally, as required to hold a phone between neck and shoulder. In addition, dealing with a lot of stress often leads to neck tension.
Finally, injury can lead to neck pain, discomfort that is sudden and severe. Car accidents and the resulting whiplash, sports collisions at speed or direct blows to the back of the head are sources of acute injury and pain. Neck injuries must be approached with caution, because an injury to the spinal cord could be involved.
Treating Neck Pain
If you experience trauma to the neck, the injury could be serious. Your neck should be immobilized until you can be moved safely and evaluated medically to ensure that there is no spinal cord injury.
Chronic conditions require ongoing treatment that may include physiotherapy, while a garden variety stiff neck should first be treated with rest and ice to prevent inflammation – apply the ice during the first 24-to-48 hours after injury.
You may also want to take over-the-counter non-steroidal anti-inflammatory medicine to relieve the pain. Afterward, you may wish to use heat on the neck to stimulate blood flow and promote healing.
To speed your recovery and prevent a recurrence of neck pain, you’ll want exercises that stretch and strengthen the muscles in your neck, shoulders and back.
A physiotherapist will be able to guide you in appropriate therapeutic exercises. Your regimen will probably include isometric exercises, where neck muscles are tightened against and opposing force, and range-of-motion exercises that work to relax and lengthen your neck muscles.
Physiotherapists also employ treatments such as ultrasound, soft tissue release and joint mobilization. To keep the neck strong and flexible over with a good range of motion, you’ll want to continue prescribed exercises on an ongoing basis.
Preventing Neck Pain
Why court discomfort? If you have been dealing with a stiff neck, no doubt you don’t want to experience another one. There are a number of measures you can take to keep it from recurring.
- At night, sleep on your side or your back, rather than on your stomach. People who sleep on their stomachs tend to twist their necks into awkward positions during the night. In addition, don’t use too many pillows in bed, because more than one pillow under your head can restrict its range of motion.
- At work, don’t sit in one position for too long; be sure to get up and move around regularly so your neck isn’t stuck in an awkward position.
- Ensure that your computer screen is at eye level so your neck isn’t tilted inappropriately; if you’re using a tablet, tilt the screen to a 45-degree angle or prop it on a pillow; if you leave it flat, your head will be bent down, stretching the ligaments.
- If you spend a lot of time on the phone, wear a headset or an earpiece to prevent awkward positioning of your head and neck.
So, don’t let your pain in the neck debilitate you. Seek the treatment you need and commit to an ongoing prevention regimen.
Let's get you some relief for your neck pain!
How to Manage a Shoulder Separation
References to shoulders generally touch upon strength: shouldering a burden requires it, as does carrying the weight of the world on your shoulders. However, those figurative tasks would be impossible to accomplish if your shoulder was in a weakened state, as it is when it’s separated.
What is a Shoulder Separation?
A shoulder separation refers to an injury to the top of the shoulder where the front of the shoulder blade (acromion) attaches to the collarbone (clavicle), forming the acromioclavicular (AC) joint. A shoulder separation, also referred to as an AC joint injury, is an injury to one or more of the four ligaments that hold the two bones together so that the bones are no longer aligned properly.
AC separations can be caused by a traumatic injury, such a blow to the site, or by repetitive overuse of the shoulder. People under 35 are the most common victims of AC joint injuries, and men are five times more likely to sustain one than women. They are often the result of a sports injury, and people in the aforementioned age group are the most usual participants in contact sports or those where collisions are likely and can produce trauma, such as football, rugby, cycling and skiing.
Overuse of the joint through repeated stress from activities such as bench-pressing heavy weights or doing physical labour with the arms raised overhead may also lead to an AC joint injury.
Grading an AC Joint Injury
Shoulder separations range from mild to severe and are graded from I to VI, depending on which ligaments are damaged and how severe the injury is. AC joint injuries graded from IV to VI generally result from high-force collisions that occur during motor vehicle crashes and must be treated surgically. Most athletes and others suffer simple AC joint injuries, Grades I, II or III.
A Grade I separation is the mildest and most common AC joint injury; the ligaments may be stretched or partially torn and the joint still lines up properly. In a Grade II dislocation, the acromioclavicular ligament is completely torn, but the ligaments at the rear of the shoulder blade, the coracoclavicular ligaments, remain attached. A Grade III separation is the most severe of the simple types and is a complete separation of the joint. All of the ligaments and the capsule surrounding the joint are torn; the shoulder sags and the clavicle is pushed up, forming a bump on the shoulder.
Symptoms of a Separated Shoulder
If you suffer an AC joint injury, you will have general shoulder pain and swelling, probably accompanied by bruising. The area above the AC joint will be especially tender and swollen and your shoulder won’t feel as strong as usual; its range of motion will also be compromised. In addition, you may have a visible bump on your shoulder and feel pain when lying on the side where the injury occurred. When you move your shoulder, you may feel a catching sensation or hear a popping sound.
Treating an AC Joint Injury
Initially, for a shoulder separation, the goal is to reduce pain by immobilizing the shoulder in a sling and applying ice to the area for 20 to 30 minutes every two hours. Your doctor may also suggest taking an over-the-counter NSAID (non-steroidal anti-inflammatory). Rest is essential during the early stages of the separation. Once the acute stage of the injury has passed, you may begin rehabilitating your shoulder with the help of a physiotherapist who will help you return to your daily and desired activities. You can expect treatment to take at least six weeks.
Your physiotherapist will create a rehabilitation plan tailored to your particular injury and to your movement goals. The plan may include:
- Strength training to strengthen the muscles in the shoulder area. Injury to the area weakens the surrounding muscles, and they must be retrained to work together properly;
- Range of motion exercises to return the joint to proper functioning as swelling and pain recede. Reaching overhead or across the body are the motions that are most often affected by a shoulder separation;
- Functional training that trains the shoulder to work properly in order for the AC joint to effectively bear the often-heavy load assigned to it; and
- Manual therapy, hands-on manipulation that mobilizes and moves your AC joint and the surrounding muscles in order to improve flexibility, motion and strength in these hard-to-reach locations.
Preventing AC Joint Injuries
Once you’ve separated your shoulder, you’ll undoubtedly want to prevent it from happening again. Exercise and stretch your shoulder muscles regularly to keep them strong and ice your shoulder after physical activity. In addition, if you experience pain during a specific activity, stop immediately. As the saying goes, “An ounce of prevention is worth a pound of cure.”
Suffering from a Shoulder Injury?
How to Avoid Accidents This Winter
As fall shades into winter, we slowly adjust to the changes in the weather: the colder temperatures, the darkness that greets us each morning and falls early each afternoon; early morning fog; fallen, slippery wet leaves; and the snow that blankets the ground and leaves roads and sidewalks slick and icy. Drivers and pedestrians both are at more risk for car accidents than usual during this time of year, and it’s not only the road conditions that make navigation challenging.
What causes accidents in the winter months?
During the fall, the sun’s glare on the roads is often noticeable and its blinding effect can also lead to accidents. Cold mornings may be accompanied by fog, making visibility challenging. There are also deer migrating and mating and they can appear on the roads unexpectedly, especially at dawn or dusk.
In winter, there may be glare from the sun shining on snow to impair visibility and there is also danger from black ice, the invisible layer of slippery stuff that blends into the sidewalk or roadway, making falls or skids increasingly likely.
Given these hazards, it is incumbent upon drivers and pedestrians both to be aware of the increased risk and to adjust their behaviours accordingly.
A 2017 study conducted by Insights West for the Insurance Corporation of British Columbia (ICBC) indicated that 75 per cent of British Columbia drivers admitted to bad driving habits and 40 per cent admitted that they may not remember all the rules of the road. However, “While they remain frustrated at the actions of others, drivers still hold their driving skills in high regard,” Mario Canseco of Insight West told Global News. “In fact, two-thirds think their skills are above average.”

Don’t take your skills for granted; drive defensively. Make sure your car is in good shape mechanically and stay focused on the road. Leave your phone alone when you’re behind the wheels and be prepared for the unexpected.
If you do get injured in an accident, remember that ICBC provides coverage for physiotherapy treatments for drivers, passengers or pedestrians that have been injured in a motor vehicle accident (MVA). For many injuries resulting from an accident, it is important to start physiotherapy as soon as possible to avoid future complications.
Fall Fixes
Weather in the fall is unpredictable, going from warm to cold at the drop of a hat. Your tires react to changes in temperature by expanding and contracting, causing them to lose pressure, so be sure to check tire pressure regularly. When fog descends, don’t turn on your high beams; they simply cause glare.

Winter Watch
As the seasons turn, prepare to switch to winter tires if you live in a region where snowfall is a regular occurrence. Why not give yourself the advantage of extra grip in slick conditions? You can’t improve the challenges the weather poses to visibility, but you can improve it by clearing your windshields before you set out and by ensuring your windshield wipers are working properly and your wiper fluid reservoir is topped up. Also, be certain that you keep your gas tank full to prevent the gas from freezing in extreme temperatures.
Pedestrian Problems
ICBC notes that 43 per cent of all crashes involving pedestrians occur between October and January. A car – because of its size and weight – is usually the victor in any interaction with a pedestrian, so, unfairly, the burden of safety falls more heavily on anyone who is walking.
In B.C., 69 per cent of accidents involving pedestrians occur at intersections, so take extra care there. Take off your headphones or earbuds so you can hear and focus on oncoming traffic; put away your phone, too, so you can focus. Keep an eye out for drivers turning both left and right through the intersection. Try to make eye contact; don’t assume that they see you.

Visibility, in fact, is a major concern, because inclement weather decreases visibility, as does darkness. As a pedestrian, don’t jaywalk, because drivers may not see you, and try to wear reflective or light-coloured clothing in the dark to give yourself added insurance when crossing streets.
Drivers, the burden may be on pedestrians to keep themselves safe, but you need to do your part. Slow down at intersections and look carefully for pedestrians. In poor weather, they may be hard to see near streetlight posts and telephone poles.
Also, at transit stops, bear in mind that they may step out into the street to look for approaching vehicles, so cut your speed. If you’re not sure whether a pedestrian plans to cross or not, a short honk and a wave can give them the go-ahead.
All-Season Security
Before you turn on your vehicle’s ignition, take a moment to think about the driving conditions and precautions you can take to ensure you arrive safely. One factor you can control is your speed. ICBC notes that speed limits are determined based on driving in ideal conditions. If you’re driving in the snow, rain or fog, slow down and allow yourself twice the usual braking distance for stopping, given the slick surfaces and poor visibility.
You should also ensure that your windshield has no streaks or smudges; the glare of oncoming headlights or the sun can magnify these distortions and impair your ability to see the road. In addition, be sure that your lights and signals are working properly and use them so that others are prepared for your next move.
Yes, accidents happen during fall and winter, but if you follow some of these tips, you’ll be less likely to be involved.
Have you been injured in a car accident?
Stay Fit During the Winter
As the days get shorter and the outdoor temperature drops, there’s no avoiding the truth: Winter is coming. Many of us dislike the combination of dark and cold and tend to huddle indoors, curling up with a book, binge-watching TV shows or eating carbs for comfort. And, once the holiday season arrives, there’s so much shopping, cooking, baking and wrapping to do that there are even more reasons to get away from our healthier warm-weather exercise routines. Add holiday parties and their rich food to the mix and you have the perfect recipe for sluggishness and inactivity.
Holiday Calories and Temptations
This year, don’t give in to all of these distractions and excuses: Resist! Your body and your mind will thank you, because you’ll be fighting back against all of those additional holiday calories you’ve consumed and you’ll be producing endorphins, the feel-good hormones, through exercise, helping you to combat the winter blues that can be triggered by lack of sunshine and Vitamin D. In addition, if you stay fit you’ll fight off the weight gain that can accompany a sedentary winter routine and will find it easy to rock that bathing suit come summer.
Outdoor Exercise
If you’ve embraced the cold weather as a component of your Canadian identity, you will undoubtedly enjoy exercising outdoors. The air is crisp, the snow is beautiful and activity brings a healthy glow to your face. Even better: While you’re in motion, you won’t feel the cool temperatures, as long as you’re dressed properly.
For cold weather activity, dressing in layers is the best approach to remaining warm and dry. You can always remove layers if you are too warm or add layers if you aren’t warm enough. The layer closest to your skin should be made of fabric that wicks away moisture; cotton isn’t ideal because once it’s damp, it remains so. The outermost layer should resist both moisture and wind.

Plan your outdoor exercise during the day, if possible, in order to take advantage of the warmer temperatures and sunshine. Exercising earlier in the day also allows you to check it off your schedule and forget about it for the remainder of the day. If your schedule only allows for exercise in the darkness, be sure to wear bright or reflective outer gear so you are visible to motorists and can stay safe.
Winter offers you the opportunity to engage in a variety of outdoors activities, so why not try a new one? Skating, sledding, snowboarding, snowshoeing and skiing are all available. There’s no need to rush out and buy equipment; rent it and take a lesson or two to test the new moves to see if they suit you. Running and walking can also be activities that help you stay fit during the winter, although they require more care – you’ll need to choose routes that are reasonably free of snow and ice and you’ll want to watch your footing more closely.
Once you’re back indoors, unless you’re wet, keep your exercise gear on for 10 to 15 minutes as your body adjusts. Losing heat from your body too rapidly can lead to post-exercise hypothermia; your body reduces its production of heat because it’s in a warm environment, but it also loses its heat stores rapidly, so don’t shock it by stripping down quickly.
Indoor Exercise
For those who don’t find the cold endearing, Canadian identities notwithstanding, there are many indoor alternatives that will help you to stay fit during the chilly, dark winter. The gym is an obvious option. Gyms are readily available, and they generally offer exercise equipment for those who prefer solo workouts, as well as classes for those who like some company as they sweat. Try yoga or Zumba or Pilates or all three, for example. There’s no need to choose solo exercise over classes or vice-versa; switch up your routine to prevent boredom. Gyms allow you to do it all.

If you are a runner or a walker, treadmills are practical indoor substitutes. Or, you may discover an indoor mall walking group; they usually meet in the morning before a mall opens, so you’ll have some exercise under your belt before the rest of your day begins.
Indoor exercise doesn’t mean investing in a gym membership if your budget doesn’t allow it. Community centres offer drop-in fees to use their facilities, which may include a pool, a running track or fitness classes. You can also get yourself a workout DVD; do yoga or an aerobics routine in the comfort of your own home. Walking stairs for a designated amount of time is also a great workout, as is dancing to the radio. Who says exercise isn’t fun?
Whether you choose to keep moving outdoors or indoors during the winter, don’t forget to stay hydrated. You might not feel as thirsty as you do in summer, but you need water just as much. If you’re out in the cold, a thermos of herbal tea is a good substitute; it keeps you warm without any diuretic effects.
Remember, no matter what type of winter exercise you choose, the goal is to continue exercising regularly. Why lose that muscle tone you’ve worked so hard to build, just because it’s cold? There’s an exercise for everyone, so no excuses!
We Can Help You Stay Fit This Winter!
Piriformis Syndrome - a real Pain in the Butt
We’ve all heard people say it, no matter how impolite it may sound, “What a pain in the butt!” However, anyone who is suffering from piriformis syndrome can make that exclamation literally: Piriformis syndrome actually can cause your buttocks to hurt.
What is Piriformis Syndrome?
Piriformis syndrome refers to the irritation to the sciatic nerve caused by the piriformis muscle.
The sciatic nerve is the body’s longest nerve, running from the base of the spine to the feet. The piriformis muscle extends from your sacrum, the triangle-shaped bone between your hipbones, across your sciatic nerve to the top of your femur, the large leg bone running from hip to knee.
This muscle helps you move your leg from side to side. When it spasms, it can put pressure on the sciatic nerve and result in a variety of symptoms.
Therefore, piriformis syndrome is actually a form of sciatica, the blanket term for any irritation of the sciatic nerve. Harvard University researchers say it is estimated that five per cent of all sciatica cases can be attributed to piriformis syndrome.
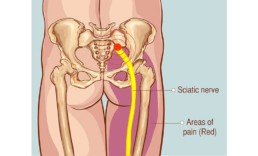
How do you treat Piriformis Syndrome?
You may find relief from pain through over-the-counter non-steroidal anti-inflammatory medications such as ibuprofen or naproxen. You can also alternate applications of ice and heat to the area in 15-minute segments, repeated every few hours to relieve your pain.
If the piriformis syndrome doesn’t disappear on its own, which it often does, the next stop is physiotherapy. Your physiotherapist will recommend a course of exercise and stretching, the mainstays of treatment for piriformis syndrome.
The physiotherapist may focus on such treatments as
- adjusting your gait;
- exercises to stretch the muscle and those surrounding it;
- improving the mobility of your sacroiliac joints;
- strengthening your hip abductor muscles, those that move your leg outward;
- acupuncture.
If your ailment doesn’t respond fully to such treatments, you may need an injection of corticosteroids to reduce muscle inflammation. An ultrasound, X-ray or other scan will help determine the proper site for such an injection to be effective.
You may also receive a transcutaneous electrical nerve stimulator treatment where a handheld device is used to send electrical charges through your skin to interrupt pain signals to the brain. In severe cases, which are very rare, surgery may be required.
What is the main cause of Piriformis Syndrome?
Piriformis syndrome can occur for a variety of reasons, including:
- prior hip surgery;
- injury;
- abnormal alignment of the spine, e.g., scoliosis;
- prolonged periods of sitting, especially if you have a wallet in your back pocket;
- a piriformis muscle or sciatic nerve that has developed abnormally;
- a discrepancy in the length of your legs;
- foot problems;
- a direct hit while playing a sport;
- a wound that reaches all the way to the muscle;
- overuse from frequent repetitive exercise, such as running;
- a change from a sedentary lifestyle to a more active one.
Symptoms of Piriformis Syndrome
Initially, piriformis syndrome may appear to be hip bursitis or a herniated disc. A catalogue of symptoms during diagnosis should make it clear to your physician that the cause of the sciatic pain is piriformis syndrome.
Individuals suffering from piriformis syndrome will have:
- trouble putting weight on one side of the buttocks;
- spasms of the piriformis muscle;
- sciatica-type pain if the hip is rotated outward when there is resistance;
- piriformis muscle pain during a rectal exam;
- difficulty sitting for long periods of time;
- pain that increases the longer you sit;
- leg and buttocks pain that increases when you are active;
- tingling or numbness in the buttocks that extends down the back of the leg.
People who sit for long periods of time on the job or at home are at risk for piriformis syndrome, as are people who regularly do rigorous lower-body workouts.
Can MRI detect Piriformis Syndrome?
Although your physician may diagnose piriformis syndrome simply based on your symptoms, he or she may also order tests to support the diagnosis. Two that have proven useful are magnetic resonance imaging (MRI), which looks for nerve inflammation, and the FAIR test (flexion, adduction and internal rotation), which stretches your hip and puts pressure on the sciatic nerve.
The test measures the delay in sciatic nerve signals during muscle compression. An MRI can also help your physician to rule out arthritis or a ruptured disc as causes of the pain.
Prevention
The stretching exercises suggested by your physiotherapist to ease your pain are also good exercises to use regularly to prevent piriformis syndrome from recurring. You should also develop good form for any repetitive motion tasks you perform regularly; consult with your physiotherapist. In addition, don’t undertake exercise that involves the injured muscles until they have healed and practise good posture, which includes wearing shoes that fit well.
Let's get you some relief!
Tailbone Pain: How can I relieve it?
The technical term for the tailbone is coccyx, which is derived from the Greek word for cuckoo. It was so named because the bone resembles the shape of the cuckoo bird’s beak. Now that we have that settled, let’s discuss tailbone pain itself. It is also known, technically, as coccydynia.
What causes Tailbone Pain?
Coccydynia is an injury to the tailbone, which is a multi-segmented bone that sits at the base of the spine immediately above the buttocks. The tailbone is small, but mighty. It helps to stabilize you when you sit and it is located in an area of the body full of tendons, muscles and ligaments.
Generally, tailbone pain sufferers experience dull, throbbing pain at the base of the spine reminiscent of a muscle spasm, but they may also feel sharp, stabbing pain when sitting for long periods of time or after being active. The pain may radiate up your back or down your legs and it may feel as if the injury is located in your tailbone itself or in the surrounding area. Sex and defecation may become painful, and women may also feel discomfort during menstruation.
Tailbone injuries have a variety of causes. A direct blow to the area that may be caused by a fall from your bicycle, for example, can result in coccydynia. Pregnancy and childbirth are also potential causes; in your last trimester of pregnancy, the ligaments in the area loosen to provide the baby with space, while a natural birth can cause trauma to the tailbone.
If you sit for long periods of time, especially if your sitting position is an awkward one or you are sitting on a hard surface like a bench, tailbone injury can result. Other potential causes include a weak pelvic floor, joint degeneration and straining due to hemorrhoids or constipation.
Tailbone Pain Treatment
Generally, coccydynia will disappear by itself in a few weeks or months. However, there’s no need to suffer unduly before the pain dissipates.
You can use over-the-counter non-steroidal anti-inflammatory medication to lessen the inflammation that is causing pain; acetaminophen, ibuprofen, naproxen or COX-2 inhibitors are helpful.
How can I relieve my Tailbone Pain?
You can ice the area immediately after the pain begins and do so for a couple of days to reduce inflammation. However, after the first few days, heat will be more helpful. Heat applied directly to the area with adhesive heat strips, a heating pad or a hot water bottle can relieve the muscle tension that causes or exacerbates the pain.
If the pain worsens during bowel movements or due to constipation, your dietary habits may require some changes. You’ll want to increase your intake of both fibre and water and you may want to consider using a stool softener.
If you are required to sit for long periods of time, a donut cushion can help relieve some of the pressure to the area; consider using one at home, at work and in the car. Whether you use one or not, make a conscious effort not to sit for long stretches of time; get up and walk around at least once an hour or consider switching to a standing desk.
Poor posture aggravates the pressure on the tailbone, so be sure to sit with your feet flat on the floor and your back against the back of the chair. When you sit down, lean forward.

Tailbone Pain Exercises and Stretches
A physiotherapist can also demonstrate ways to help reduce your pain and prescribe a suitable course of exercises that will alleviate tension and strengthen the surrounding muscles, including the stomach and the pelvic floor.
Once movement is less painful, your physiotherapist may recommend gentle aerobic activity to increase the blood flow to the area to promote healing. Aerobic exercise also stimulates the release of endorphins, which are your body’s natural pain-relieving chemicals.
A physician may suggest gentle massage to the muscles attached to the tailbone. He or she might also inject a local anesthetic into the tailbone to relieve pain for a few weeks.
Surgery to remove the tailbone is a last resort and won’t be suggested until all other avenues of treatment are exhausted.
If you have severe, unrelenting pain that persists, you shouldn’t ignore it; there may be a more serious underlying cause. Your physician will want to conduct diagnostic tests, such as X-rays or an MRI, to determine if tumours, cysts or bone spurs are causing the coccydynia.
Remember, it’s the tail that wags the dog, so to speak. If your tailbone hurts, you’ll feel like growling instead, so get treatment.




























